Antibiotic Overuse: How Misuse Fuels Resistance and C. difficile Infections
 Jan, 15 2026
Jan, 15 2026
Every time you take an antibiotic when you don’t need it, you’re not just helping yourself-you’re helping bacteria become stronger. That’s the harsh truth behind the growing crisis of antibiotic overuse. It’s not just about one bad pill or one unnecessary prescription. It’s about a global pattern that’s turning once-treatable infections into life-threatening ones-and making Clostridioides difficile (C. difficile) outbreaks more common than ever.
What Happens When Antibiotics Don’t Work Anymore?
Antibiotics were once miracles. A simple infection like a urinary tract infection or a strep throat could be cleared in days. Today, that’s not guaranteed. According to the World Health Organization’s 2025 global report, one in six bacterial infections worldwide are now resistant to standard antibiotics. That means the drugs doctors reach for first often don’t work anymore. This isn’t magic. It’s evolution. Bacteria don’t sit still. When exposed to antibiotics too often-or too lightly-they adapt. They develop defenses. They mutate. They survive. And then they pass those defenses to their offspring. Over time, entire strains become untouchable by the drugs we rely on. The most dangerous resistance patterns are showing up in common pathogens: Escherichia coli, Klebsiella pneumoniae, and Staphylococcus aureus. In some places, 42% of E. coli infections no longer respond to third-generation cephalosporins. In others, 35% of S. aureus cases are methicillin-resistant (MRSA). These aren’t rare cases. They’re the new normal in hospitals and communities alike. And it’s getting worse. Between 2018 and 2023, resistance increased in over 40% of the antibiotic-pathogen combinations tracked globally. Last-resort drugs like carbapenems-used when everything else fails-are losing their power. Experts warn that by 2035, resistance to these final options could double compared to 2005 levels.C. difficile: The Hidden Consequence of Antibiotic Misuse
One of the most dangerous side effects of antibiotic overuse isn’t resistance-it’s disruption. Your gut is full of good bacteria. They help digest food, train your immune system, and keep harmful microbes in check. When you take antibiotics, especially broad-spectrum ones, you don’t just kill the bad bugs. You wipe out the good ones too. That’s when Clostridioides difficile (C. difficile) moves in. It’s a tough, spore-forming bacterium that thrives when the gut microbiome is empty. Once it takes hold, it causes severe diarrhea, colitis, and in extreme cases, toxic megacolon or death. The CDC estimates that in the U.S. alone, C. difficile causes nearly half a million infections each year. While exact global numbers are harder to track, the pattern is clear: more antibiotics = more C. difficile. What’s worse? C. difficile doesn’t just appear after one course of antibiotics. It’s often triggered by repeated or prolonged use. Someone on multiple rounds of antibiotics for recurring sinus infections, bronchitis, or even acne is at much higher risk. And once you’ve had a C. difficile infection, your chances of getting it again jump dramatically. Recovery isn’t just about killing the bug-it’s about rebuilding your gut. And that can take months.Why Are We Still Overprescribing?
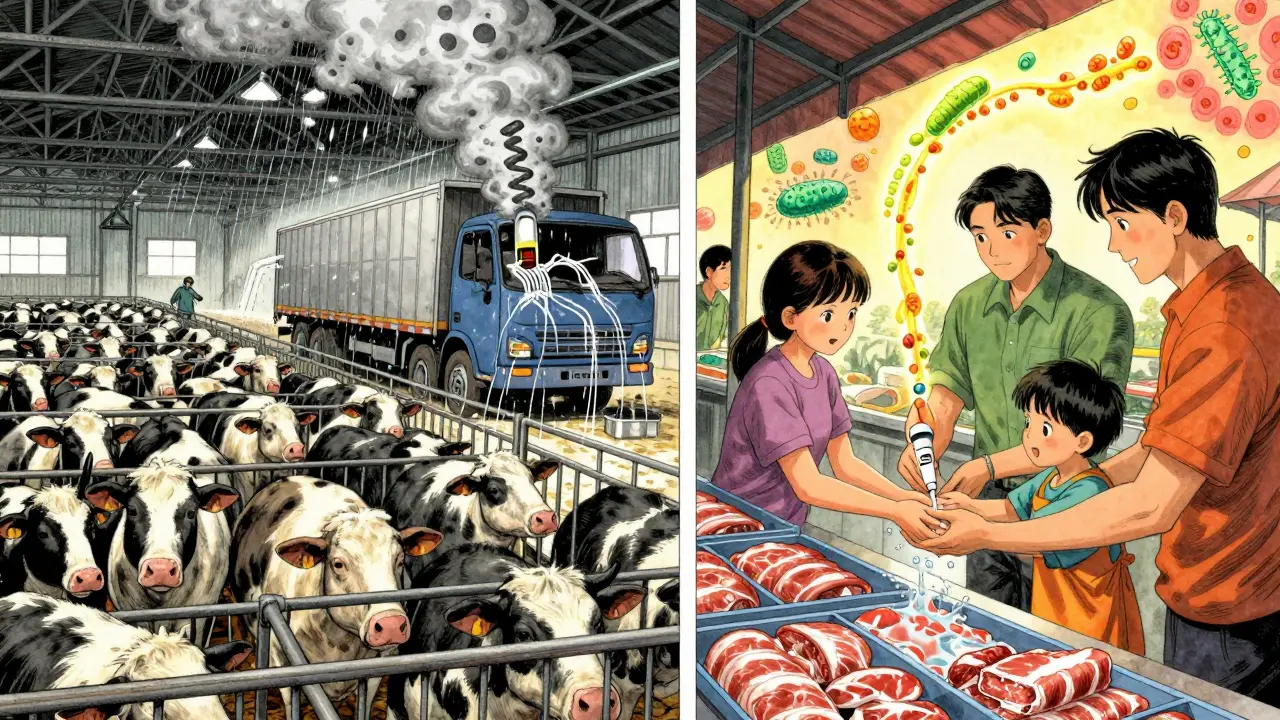
You might wonder: if the risks are so clear, why are doctors still giving out antibiotics like candy? Part of it is pressure. Patients show up with a cough, a sore throat, or a runny nose-and they want a pill. They’ve seen antibiotics fix things before. They don’t understand that 70% of colds and most sore throats are caused by viruses. Antibiotics don’t touch viruses. But telling someone “no” feels like letting them down. Doctors are caught in the middle. In busy clinics, with limited time and no rapid tests, it’s easier to write a prescription than to explain why it won’t help. And in some places, especially where diagnostics are scarce, doctors have no choice but to guess. If a patient has a fever and a cough, they get antibiotics-just in case. Then there’s agriculture. Nearly 70% of all antibiotics produced globally are used in livestock-not to treat sick animals, but to make them grow faster and prevent disease in crowded, unsanitary conditions. These drugs don’t stay in the barn. They end up in our water, our soil, and our food. Resistant bacteria from farms spread to humans through meat, water runoff, and even dust in the air.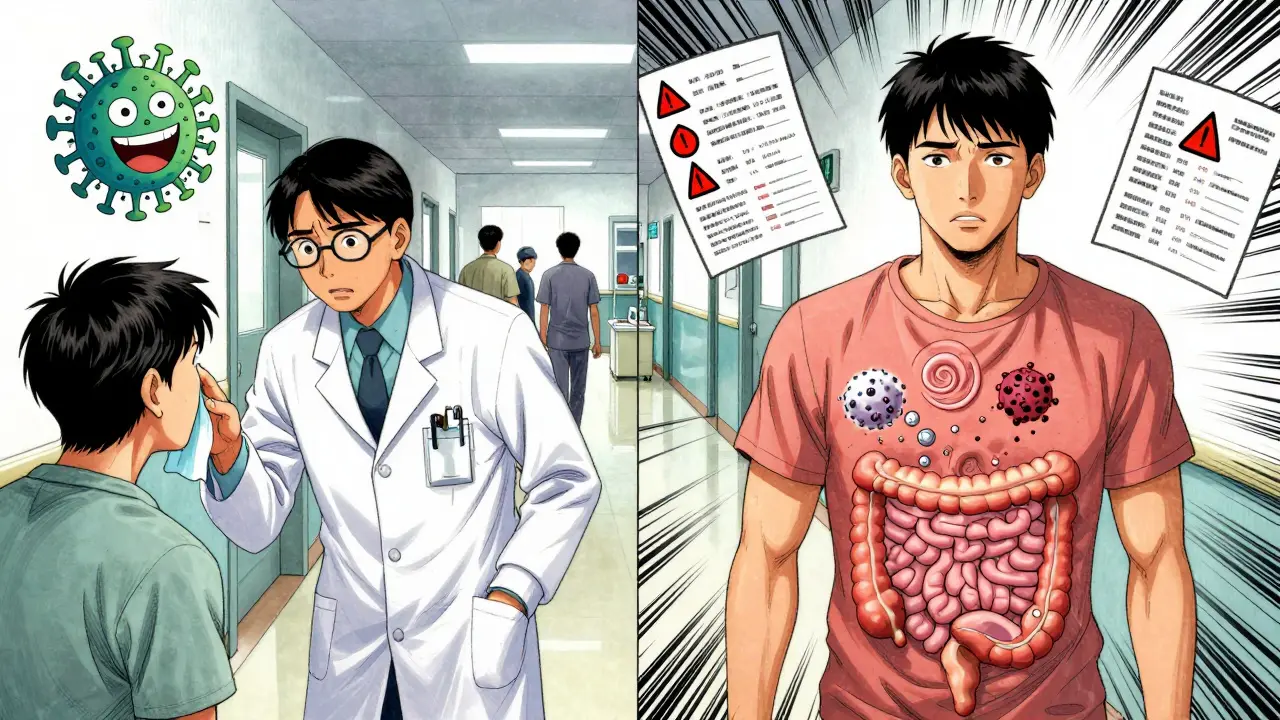
The Human Cost Is Already Here
This isn’t a future threat. It’s happening now. In 2019, antimicrobial resistance directly caused 1.27 million deaths worldwide. It contributed to another 4.95 million. That’s more than HIV/AIDS or malaria. By 2050, if nothing changes, AMR could kill 10 million people a year-more than cancer. Doctors are seeing it in real time. Patients who used to recover from a kidney infection in a week now need weeks of IV antibiotics. Some don’t respond at all. There are cases where clinicians run out of options. No drug works. No backup. No cure. That’s not science fiction. It’s clinical reality. The COVID-19 pandemic made it worse. During the peak years, antibiotic use surged by 30% in hospitals, even though most patients had viral infections. As a result, resistant infections rose by 20% in U.S. healthcare settings between 2020 and 2022. Progress made over the past decade-like fewer hospital-acquired MRSA cases-was wiped out in just two years.What Can You Do?
You don’t need to wait for governments or pharmaceutical companies to fix this. You have power too.- Don’t demand antibiotics. If your doctor says it’s a virus, believe them. Ask: “Is there a test to confirm this is bacterial?”
- Never share or save antibiotics. Taking leftover pills from a friend’s prescription is dangerous. You might not be taking the right drug, the right dose, or for the right length of time. That’s how resistance starts.
- Finish your full course-if you really need it. Stopping early when you feel better leaves behind the toughest bacteria. They’re the ones that survive and multiply.
- Choose meat raised without routine antibiotics. Look for labels like “raised without antibiotics” or “organic.” Your choices shape the market.
- Practice good hygiene. Wash your hands. Get vaccinated. Prevent infections before they start.

Sarah Mailloux
January 15, 2026 AT 14:28Amy Ehinger
January 17, 2026 AT 12:02Crystel Ann
January 18, 2026 AT 18:20Niki Van den Bossche
January 19, 2026 AT 00:01Jan Hess
January 19, 2026 AT 07:29Iona Jane
January 19, 2026 AT 08:18Jaspreet Kaur Chana
January 20, 2026 AT 16:02Haley Graves
January 20, 2026 AT 20:44ellen adamina
January 21, 2026 AT 15:32