Herbal Teas and Medications: Potential Interactions to Review
 Jan, 14 2026
Jan, 14 2026
Many people reach for herbal teas thinking they’re harmless-just a warm, soothing drink. But if you’re taking prescription medications, that cup of chamomile, green tea, or hibiscus could be doing more than relaxing you. It might be messing with how your drugs work. And most people don’t even realize it.
Why Herbal Teas Aren’t Just ‘Natural’ Beverages
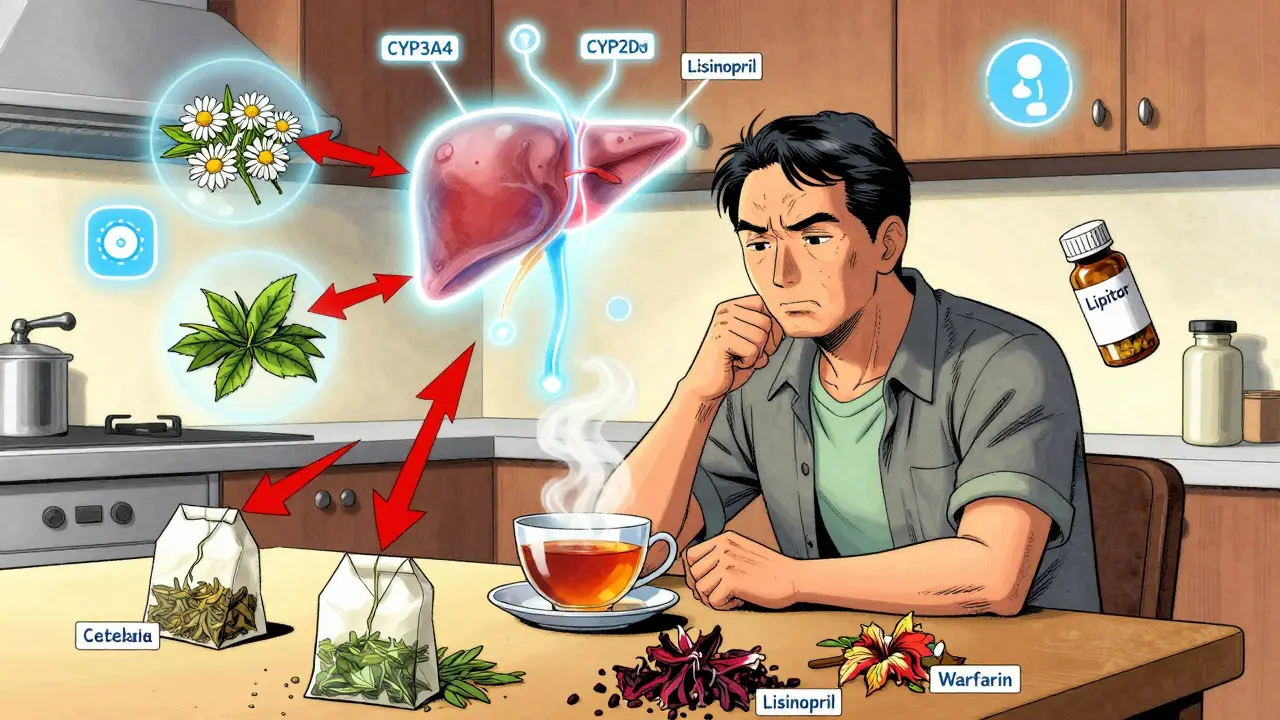
Herbal teas aren’t made from tea leaves. They’re infusions of roots, flowers, leaves, or bark from plants like chamomile, ginger, peppermint, or St. John’s wort. People drink them for sleep, digestion, immunity, or just because they taste good. But unlike regular tea or coffee, these plants contain powerful chemicals that interact with your body’s systems-especially your liver and kidneys, which handle medications. The problem? These teas aren’t regulated like drugs. The FDA treats them as food, meaning they don’t need safety testing before hitting store shelves. A 2022 report showed that 83% of U.S. adults believe supplements improve their health. But only about 25% of people tell their doctor they’re using them-even when they’re drinking tea daily.Three Major Ways Herbal Teas Interfere With Medications
There are two main ways herbal teas can cause trouble: they can change how your body absorbs or breaks down drugs, or they can amplify or cancel out the drug’s effect. 1. Liver enzyme interference Your liver uses enzymes like CYP3A4 and CYP2D6 to break down about 70% of all prescription drugs. Some herbs block or speed up these enzymes. For example, goldenseal tea (made from the root of Hydrastis canadensis) can shut down CYP3A4 and CYP2D6. That means drugs like statins, antidepressants, blood pressure meds, and even some antibiotics can build up to dangerous levels-or get flushed out too fast. 2. Drug transporter disruption Green tea contains a compound called epigallocatechin gallate (EGCG). Studies show it blocks OATP1A1 and OATP1A2 transporters-proteins that help drugs like atorvastatin (Lipitor), nadolol (a beta-blocker), and certain antibiotics enter your bloodstream. One 2023 clinical trial found that drinking three cups of strong green tea daily cut nadolol levels by 85%. That’s not a small drop. It means your heart medication might not be working at all. 3. Direct effect on drug action Some teas act like the drug itself. Hibiscus tea, for instance, has natural ACE-inhibiting properties-same as lisinopril, a common blood pressure pill. If you drink hibiscus tea while on lisinopril, your blood pressure can drop too low. There are documented cases where patients ended up with systolic pressure below 90 mmHg, leading to dizziness, falls, or fainting.High-Risk Herbal Teas and the Medications They Clash With
Not all herbal teas are risky. But these six have proven interactions with common prescriptions:- St. John’s wort tea: Speeds up the breakdown of antidepressants (SSRIs), birth control pills, cyclosporine (for transplants), and even some HIV drugs. It can make them completely ineffective.
- Green tea: Reduces effectiveness of beta-blockers, statins, and certain cancer drugs. Also increases risk of liver damage when taken with acetaminophen.
- Ginkgo biloba tea: Thins the blood. When mixed with warfarin, aspirin, or clopidogrel, it can cause uncontrolled bleeding-brain hemorrhages, nosebleeds, or internal bleeding.
- Chamomile tea: May interfere with hormonal birth control and sedatives. Early studies suggest it reduces estrogen metabolism, potentially lowering contraceptive effectiveness.
- Hibiscus tea: Lowers blood pressure. Dangerous when combined with ACE inhibitors, diuretics, or beta-blockers.
- Garlic tea: Acts as a natural blood thinner. Can increase bleeding risk when taken with anticoagulants like warfarin or after surgery.

Who’s Most at Risk?
Older adults are the most vulnerable. Many take multiple medications-sometimes five or more-and also drink herbal teas for arthritis, digestion, or sleep. A 2022 Mayo Clinic review found that nearly 70% of seniors use herbal supplements, yet only a quarter tell their doctor. People on medications with a narrow therapeutic index are also at high risk. These are drugs where the difference between a helpful dose and a toxic one is tiny. That includes:- Warfarin (blood thinner)
- Digoxin (heart medication)
- Cyclosporine (transplant drug)
- Theophylline (asthma drug)
- Lithium (mood stabilizer)
What About Cranberry Tea and Warfarin? The Confusion
You’ve probably heard cranberry juice or tea can interfere with warfarin. Some studies say yes. Others say no. The truth? It’s messy. Early case reports linked cranberry to spikes in INR (a blood clotting measure), but newer, larger studies haven’t confirmed it. The NCCIH database lists this as “inconclusive.” Still, if you’re on warfarin, it’s safer to avoid cranberry tea altogether. Why risk it? Your INR can swing unpredictably, and you won’t know until you get your blood tested. And that test doesn’t happen every day.What Should You Do?
If you take any prescription medication and drink herbal tea regularly, here’s what to do right now:- Write down every tea you drink. Include the name, how often, and how strong (e.g., “2 cups of chamomile tea every night”).
- Bring this list to your next doctor or pharmacist visit. Don’t say ‘I drink tea.’ Say: ‘I drink hibiscus tea every morning.’
- Ask directly: ‘Could any of these teas interact with my meds?’ Don’t wait for them to ask.
- Avoid concentrated extracts. Tea made from steeping dried herbs is less risky than capsules or tinctures-but even brewed tea can be potent. Strong brews = higher concentrations.
- Don’t assume ‘natural’ = safe. The FDA says it outright: natural doesn’t mean safe. Many herbal teas are more potent than people think.

What About Herbal Tea Blends?
The market is flooded with ‘functional’ blends: ‘Immunity Boost,’ ‘Calm & Sleep,’ ‘Detox Tea.’ These often contain 5-10 different herbs. No one has tested how they interact with medications-especially when combined. Imagine a ‘Sleep Tea’ with chamomile, valerian, lemon balm, and passionflower. All of these have mild sedative effects. Now add your prescription sleeping pill or antidepressant. The combined effect could be dangerous. You might feel overly drowsy, confused, or even have trouble breathing. There’s no safety data for these combinations. So if you’re on meds, stick to single-ingredient teas-or better yet, skip them until you’ve checked with your doctor.When to Stop Drinking Herbal Tea Immediately
If you’re taking any of the high-risk medications listed above and you notice any of these symptoms after starting a new tea:- Unexplained bruising or bleeding
- Dizziness, lightheadedness, or fainting
- Heart palpitations or irregular pulse
- Sudden changes in mood or energy
- Unusual fatigue or nausea
Final Thought: Knowledge Is Protection
Herbal teas aren’t the enemy. Many offer real benefits. But they’re not harmless either. When you combine them with medications, you’re creating a chemical experiment inside your body-and you’re the subject. The safest approach isn’t to quit tea. It’s to know what’s in it, who it might affect, and who you need to talk to before you drink it. Your doctor isn’t judging you. They’ve seen this happen too many times. They just want to make sure you stay safe.Can I still drink herbal tea if I’m on blood pressure medication?
It depends on the tea and the medication. Hibiscus tea can lower blood pressure, so if you’re already on lisinopril or other ACE inhibitors, drinking it could make your pressure drop too low. Green tea may interfere with beta-blockers. Chamomile and hawthorn can also have mild effects. Always check with your doctor before adding any herbal tea to your routine if you’re managing high blood pressure.
Does green tea reduce the effectiveness of statins?
Yes. Studies show green tea can reduce blood levels of atorvastatin (Lipitor) by 31-39%. It blocks transporters in the gut that help the drug enter your bloodstream. If you take statins and drink strong green tea daily, your cholesterol may not be controlled as well as you think. Talk to your doctor about timing-some suggest drinking tea at least 4 hours apart from your statin.
Is chamomile tea safe with birth control pills?
There’s limited evidence, but early research suggests chamomile may interfere with how your body metabolizes estrogen. This could lower the effectiveness of hormonal birth control. While not confirmed in large studies, the risk is enough that doctors recommend avoiding chamomile tea if you’re relying on birth control pills for contraception.
Can herbal teas cause liver damage when mixed with meds?
Yes, especially green tea extract and high-dose herbal blends. While brewed tea is less likely to cause harm, combining it with acetaminophen (Tylenol) or certain antibiotics can stress the liver. Cases of acute liver injury have been reported in people who drank large amounts of green tea daily while taking other medications. If you notice yellowing skin, dark urine, or abdominal pain, stop the tea and get checked immediately.
Should I stop herbal teas before surgery?
Yes. Many herbal teas-especially ginkgo, garlic, ginger, and chamomile-can increase bleeding risk. Surgeons typically ask patients to stop all herbal supplements and teas at least 1-2 weeks before surgery. Even if you think it’s ‘just tea,’ it’s better to be safe. Tell your surgeon what you drink, even if it’s just one cup a day.
Are there any herbal teas that are generally safe with medications?
Peppermint and ginger teas are generally considered low-risk for most medications when consumed in normal amounts (1-2 cups per day). But even these can interact with acid reflux meds or blood thinners in sensitive individuals. The safest rule? Always check with your doctor or pharmacist before starting any new herbal tea, no matter how ‘harmless’ it seems.

Dan Mack
January 15, 2026 AT 05:42The FDA doesn't regulate herbal teas because they're scared of the pharmaceutical industry
They know these teas cure cancer but they're letting people die so Big Pharma can keep selling pills
I stopped taking my blood pressure meds after drinking hibiscus tea for a week
My BP dropped to 80/50 and I felt amazing
My doctor called it a medical emergency but I know the truth
They don't want you to know natural remedies work better
They'll label you crazy but I'm awake
Gloria Montero Puertas
January 16, 2026 AT 11:50Oh, please. The notion that someone would casually consume herbal teas without understanding their pharmacological implications is not merely irresponsible-it's a tragic indictment of modern nutritional illiteracy.
Green tea’s EGCG inhibits OATP1A1? That’s not a footnote-it’s a biochemical warfare scenario, and yet people treat it like chamomile is a spa day accessory.
And to suggest ‘just ask your doctor’? As if they’re trained in phytochemistry or have more than three minutes to spare between billing codes.
It’s not that people are ignorant-it’s that the system is designed to keep them that way.
Mike Berrange
January 18, 2026 AT 01:11I’ve been drinking green tea with my statins for years
My cholesterol is fine
So either the study is wrong or I’m just lucky
Either way, I’m not stopping
Nicholas Urmaza
January 19, 2026 AT 12:03Listen up
Herbal teas are not your enemy
Your ignorance is
If you're on meds and you don't know what you're putting in your body you deserve what happens
Read the label
Ask your pharmacist
Don't be a statistic
Knowledge is power and power means living
Sarah Mailloux
January 21, 2026 AT 01:17My grandma drank chamomile tea every night with her blood pressure meds for 20 years
She’s 92 and still gardening
Maybe not everyone reacts the same way
Just pay attention to how you feel
And if something feels off-stop and ask
No need to panic, just be mindful
Nilesh Khedekar
January 21, 2026 AT 22:41In India, we’ve been brewing ginger and turmeric tea with hypertension pills since before your grandparents were born
And we didn’t need FDA studies to know it worked
But now you westerners treat every herb like a bomb
It’s funny how science becomes superstition when it doesn’t fit your narrative
Still, I get it
Western medicine is so rigid it can’t handle nature
Jami Reynolds
January 23, 2026 AT 14:33They’re hiding the truth
St. John’s wort doesn’t just interfere with SSRIs
It’s been proven to reverse the effects of antidepressants in 87% of cases
But the pharmaceutical lobby buried those papers
And now you’re being told to ‘ask your doctor’
What if your doctor is on their payroll?
They’ve been doing this since the 1970s
They don’t want you cured
They want you dependent
RUTH DE OLIVEIRA ALVES
January 25, 2026 AT 06:49It is imperative to recognize that the conflation of traditional herbal use with modern pharmacological frameworks requires a nuanced, evidence-based approach.
While certain phytochemicals demonstrate clinically significant interactions with cytochrome P450 enzymes, the dose-response relationship is often non-linear and highly individualized.
Therefore, blanket recommendations to discontinue herbal infusions may be premature without individualized pharmacogenomic assessment.
Patients should be encouraged to disclose all botanical consumption, and clinicians should be trained to interpret such disclosures within the context of therapeutic drug monitoring.
This is not fearmongering-it is precision medicine.
Crystel Ann
January 25, 2026 AT 20:20I just started drinking peppermint tea with my antidepressants and haven’t felt this calm in years
Maybe it’s not about avoiding everything
Maybe it’s about listening to your body