How to Prevent Wrong-Patient Errors at the Pharmacy Counter
 Feb, 9 2026
Feb, 9 2026
Imagine walking up to the pharmacy counter, handing over your prescription, and walking out with someone else’s medicine. It sounds impossible - but it happens more often than you think. In community pharmacies across the U.S. and UK, wrong-patient errors occur when a medication is accidentally given to the wrong person. These aren’t just minor mix-ups. They can lead to dangerous drug interactions, allergic reactions, or even death. The good news? Wrong-patient errors are almost always preventable. And the best pharmacies are proving it every day.
Why Wrong-Patient Errors Happen
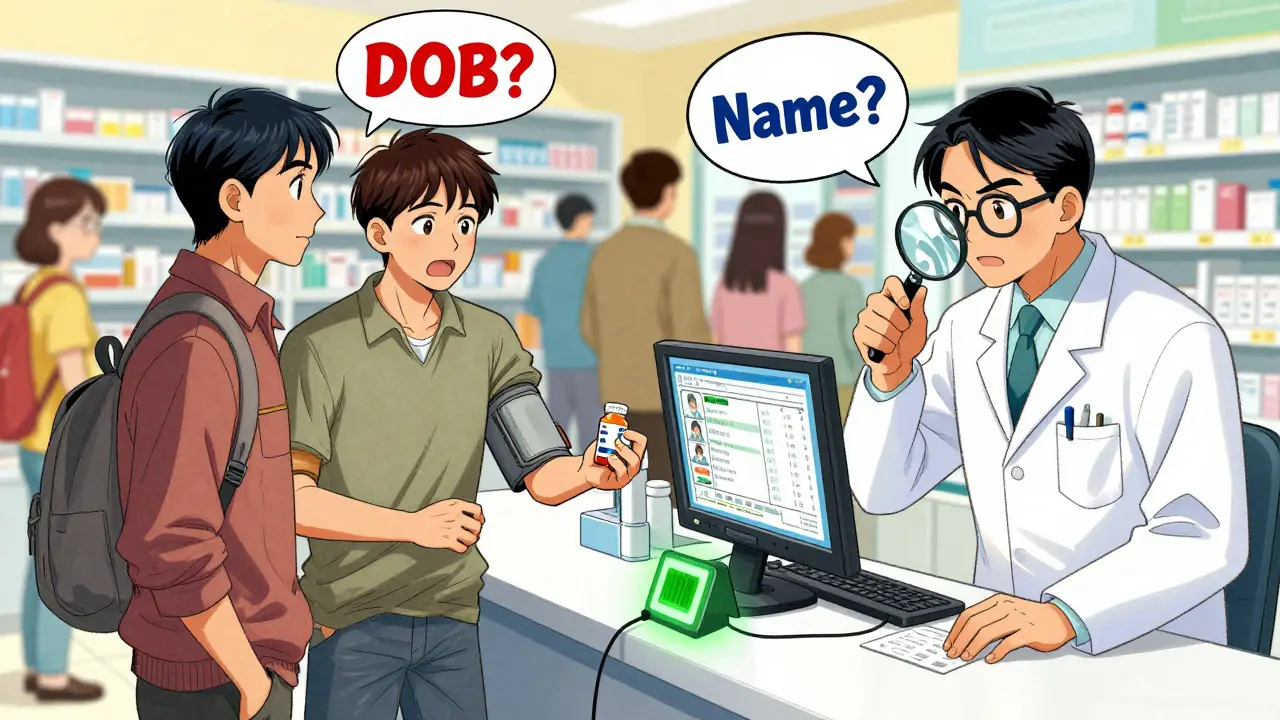
These mistakes don’t happen because pharmacists are careless. They happen because the system is fragile. During busy hours, staff juggle dozens of prescriptions, ringing up customers, answering questions, and managing insurance issues. A patient named John Smith picks up his blood pressure med. Minutes later, another John Smith - same first name, same last name, same birthday - comes in for his antibiotic. One slip. One misread. One wrong bag handed over. According to the Institute for Safe Medication Practices (ISMP), nearly 22% of wrong-patient errors involve patients with similar names - what experts call "sound-alike, look-alike" cases. Elderly patients, non-English speakers, or those with memory issues are especially vulnerable. And when staff are rushed, they sometimes skip steps they’ve done a thousand times before.The Two-Step Verification Rule
The simplest, most powerful tool to stop these errors is the two-identifier rule. Every pharmacy should verify two things before handing over any prescription:- Full legal name
- Date of birth
Barcode Scanning: The Game-Changer
Manual checks help - but they’re not enough. The real breakthrough came with barcode scanning. Today, leading pharmacies like Walgreens and Kroger Health use handheld scanners that read both the prescription label and a patient’s ID card or pharmacy membership card. The system won’t let the transaction complete unless both barcodes match perfectly. Walgreens rolled this out across 9,000+ locations in 2021. Within 18 months, wrong-patient errors dropped by 63%. Kroger Health went even further. Since launching their full safety program in 2022 across 2,200 pharmacies, they’ve reported zero wrong-patient errors for 18 straight months. The technology isn’t magic - it’s math. A barcode has unique data tied to a specific patient and prescription. If the system says “No Match,” the medication stays locked until the issue is cleared. No guesswork. No shortcuts.
RFID and Biometrics: The Future Is Here
Some pharmacies are already moving beyond barcodes. Radio Frequency Identification (RFID) wristbands - common in hospitals - are now being tested in outpatient settings. A 2023 study found a 78% reduction in errors when RFID was paired with barcode scanning. Even more advanced? Fingerprint verification. Walgreens piloted fingerprint scans in 500 stores in January 2025. Initial results showed 92% accuracy. Patients simply place a finger on a reader - no card, no ID, no memory needed. But privacy concerns have slowed full adoption. Still, the trend is clear: biometrics are coming. AI-powered facial recognition and voice identification are also in development. Experts predict that by 2027, 70% of pharmacies will use some form of automated patient verification. The goal? Near-zero errors.The Human Factor: Counseling as a Final Safety Net
Technology helps - but people save lives. When a pharmacist takes two minutes to review the medication with the patient, errors often catch themselves. Pharmacy Times found that 83% of dispensing mistakes are caught during counseling. A patient might say: “I don’t take this pill.” Or, “My doctor said this was for my back pain, not my diabetes.” These moments are priceless. That’s why the best pharmacies train staff to ask open-ended questions: “What’s this medication for?” “Have you taken it before?” “Any side effects you’ve noticed?” It’s not about suspicion. It’s about partnership. Patients aren’t just customers - they’re active participants in their own safety.
Why Some Pharmacies Still Struggle
Not all pharmacies can afford high-tech systems. Independent pharmacies, especially small ones, face real barriers. Barcode scanners, software integration, and staff training cost between $15,000 and $50,000. For a single-location shop, that’s a huge investment. A 2024 ASHP survey found that only 42% of independent pharmacies use barcode scanning. The rest rely on manual checks - which, without strict discipline, leave gaps. There’s also pressure from patients. About 22% of people find repeated ID checks annoying - especially older adults who’ve been going to the same pharmacy for decades. But when staff explain why it matters - “This is to make sure you get the right medicine, not someone else’s” - resistance drops.What You Can Do as a Patient
You don’t have to wait for the pharmacy to fix this. You can help.- Always carry your ID and insurance card - even if you’ve been there for years.
- Speak up if you’re asked for your DOB. Say it clearly. Don’t assume they already know.
- Ask: “Is this my prescription?” before leaving the counter.
- If the pill looks different than last time, ask why.
- Report any confusion or mistakes - even if nothing bad happened. Your feedback helps.
The Bottom Line: Safety Is a System, Not a Checklist
Wrong-patient errors aren’t about one bad day or one tired technician. They’re about a system that’s too easy to break. The solution isn’t more training - it’s better design. The most effective pharmacies use a three-part approach:- Standardized protocols - always verify name and DOB.
- Technology - barcode or RFID scanning to block errors before they happen.
- Empowered staff - anyone can stop the process if something feels off.
What are the most common causes of wrong-patient errors at the pharmacy?
The most common causes are similar patient names (like John Smith vs. John Smith), rushed conditions during peak hours, skipping verification steps, and reliance on memory instead of written checks. About 22% of errors involve patients with identical or very similar names. Technology gaps and lack of standardized protocols in smaller pharmacies also contribute significantly.
Can I refuse to give my date of birth at the pharmacy?
You can, but the pharmacy may refuse to dispense your medication. Since 2024, the National Association of Boards of Pharmacy (NABP) requires dual-identifier verification (name and date of birth) for all prescriptions. This is a safety standard, not a privacy invasion. If you’re uncomfortable, ask why it’s needed - most pharmacists will gladly explain how it prevents life-threatening mistakes.
Do all pharmacies use barcode scanning to prevent errors?
No. Large chain pharmacies like CVS, Walgreens, and Kroger use barcode scanning in nearly all locations. But many independent pharmacies still rely on manual checks due to cost. As of 2024, only 42% of independent pharmacies have adopted barcode systems. The technology is proven - but not yet universal.
How effective is patient counseling in catching errors?
Extremely effective. According to Pharmacy Times, 83% of dispensing errors are caught during counseling - the final conversation between the pharmacist and patient before leaving the counter. Questions like “What’s this for?” or “Have you taken this before?” often reveal mismatches that no system caught. Never skip this step.
What should I do if I think I received someone else’s medication?
Stop. Don’t take it. Don’t leave the pharmacy. Tell the pharmacist immediately. Say: “I think this might be someone else’s prescription.” They’ll stop the process, check the records, and correct it. Most errors are caught before the patient leaves - but only if someone speaks up. Your voice saves lives.
Are wrong-patient errors becoming less common?
Yes - but slowly. Pharmacies that use technology and strict protocols have cut errors by 60-89%. However, without nationwide adoption of barcode systems and standardized verification, progress is uneven. The goal of organizations like the Pharmacy Quality Alliance is zero wrong-patient errors by 2030. That’s possible - but only if every pharmacy invests in safety.

John Sonnenberg
February 10, 2026 AT 13:19The system is broken and everyone knows it. Pharmacies treat patients like inventory. I’ve been to three different stores in the last month and each time they skipped the DOB check. Not because they forgot. Because they’re tired of the paperwork. And now? I’m the one who has to remind them. I don’t want to be the enforcer. I just want my damn medication without becoming a human barcode scanner.
PAUL MCQUEEN
February 12, 2026 AT 00:16Interesting how they mention CVS and Walgreens like they’re saints. Meanwhile, the real issue is that pharmacies are understaffed and overworked. The tech is nice, but if you’re running on three people during peak hours, no amount of barcode scanning will fix human exhaustion. Also, why is no one talking about the fact that most patients don’t even know their own DOB? I’ve seen grandmas fumble with it for five minutes. The system assumes competence where none exists.
Monica Warnick
February 12, 2026 AT 12:14I work in a small independent pharmacy. We don’t have barcode scanners. We can’t afford them. We do manual checks. We say the name. We say the DOB. We look at the ID. We double-check the prescription. And yes, we’ve had errors. One time, a woman got her husband’s antibiotics. She didn’t notice until she started vomiting. We fixed it. But we lost her as a customer. She said we were ‘too slow.’ We’re not slow. We’re careful. And now? We’re trying to get funding. But nobody cares until someone dies. And then? They’ll blame the pharmacist.
Ashlyn Ellison
February 12, 2026 AT 18:34Just got my script filled today. Pharmacist asked for my DOB. I said it. She scanned my card. Then she looked me in the eye and said, ‘You’re not supposed to take this with grapefruit juice.’ I didn’t even know that. She didn’t have to. But she did. That’s the difference. Tech helps. But the person behind the counter? That’s the real safety net.
Jonah Mann
February 14, 2026 AT 09:41barcods r the future but i gotta say i hate when they make you pull out ur id every time. i’ve been going to this same pharmacy since 2010. they know me. they know my meds. why do i need to prove i’m me again? also i think they should use voice recognition. like say your name and it matches. no card. no id. just talk. its 2025. we’re not in 2005. also typo on the label once. almost got someone else’s blood thinner. scary stuff.
THANGAVEL PARASAKTHI
February 16, 2026 AT 07:29As someone from India where pharmacy systems are still catching up, I see this as a global issue. In my country, we rely on handwritten prescriptions and memory. I’ve seen patients get the wrong medicine. But here’s the thing: community trust matters more than tech. If the pharmacist knows you, your family, your history - they’ll catch the error before it happens. Technology is great, but human connection is the original safety protocol. Maybe we don’t need to copy the U.S. model exactly. We need context-sensitive solutions.
Chelsea Deflyss
February 17, 2026 AT 09:59Wow. So now we’re going to scan fingerprints? Next thing you know, they’ll be implanting chips. This isn’t safety. This is surveillance dressed up as care. I don’t want a pharmacy that treats me like a criminal just because I’m trying to get my diabetes meds. If you’re so worried about errors, train your staff. Don’t turn every visit into a TSA checkpoint. I’m not a threat. I’m a person.
Tricia O'Sullivan
February 19, 2026 AT 00:36While I appreciate the technological advancements outlined in this article, I must express my concern regarding the erosion of patient autonomy in the name of procedural compliance. The requirement for dual verification, while statistically sound, may inadvertently cultivate a culture of compliance over communication. A respectful, patient-centered approach - wherein the pharmacist engages in a brief, empathetic dialogue - may yield comparable safety outcomes without the perceived intrusion. The human element, when cultivated with dignity, remains indispensable.
Scott Conner
February 19, 2026 AT 07:26Wait, so if I’m 78 and I forget my DOB, do they just refuse to give me my meds? That seems harsh. What if I have dementia? What if I’m confused? The system assumes everyone is cognitively capable. But not everyone is. There’s got to be a better way than just saying ‘no’ to people who can’t remember. Maybe a family member verification? Or a trusted contact? This feels like a solution that works for young, tech-savvy people - but leaves others behind.
Andrew Jackson
February 20, 2026 AT 00:21Let’s be honest: America’s healthcare system is a joke. We spend trillions on drugs, but we can’t even make sure the right person gets the right pill? This isn’t about technology. This is about moral decay. We’ve outsourced responsibility. We’ve automated humanity. And now we’re surprised when people die? This is what happens when you let corporations run medicine. Fix the system. Not the scanner. Stop treating patients like numbers. Start treating them like citizens. This isn’t innovation - it’s desperation.