Stroke Types: Ischemic vs. Hemorrhagic and How to Prevent Them
 Jan, 9 2026
Jan, 9 2026
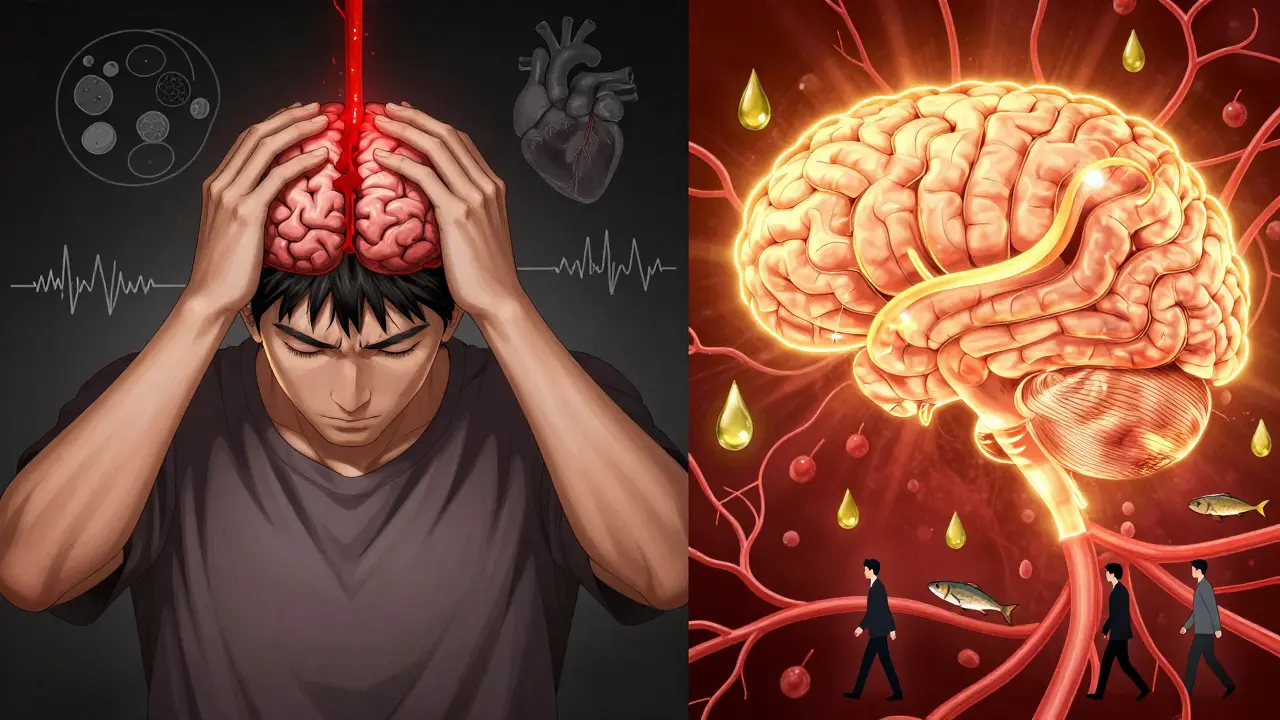
What Exactly Is a Stroke?
A stroke happens when the brain doesn’t get enough oxygen because blood flow is cut off or interrupted. It’s not a heart attack, but it’s just as urgent. Every minute without blood flow kills nearly 2 million brain cells. That’s why recognizing the signs fast can mean the difference between full recovery and permanent disability-or death.
There are two main types: ischemic and hemorrhagic. Together, they make up nearly all strokes. Knowing the difference isn’t just medical jargon-it affects how you respond, what treatments you get, and how you prevent it from happening again.
Ischemic Stroke: The Blocked Artery
Eighty-seven out of every 100 strokes are ischemic. That means something is blocking blood flow to your brain. Most often, it’s a clot. These clots can form in two ways: either right inside a brain artery (thrombotic stroke), or they travel from somewhere else-like your heart-into the brain (embolic stroke).
Thrombotic strokes are often tied to plaque buildup in larger arteries, especially if you have high cholesterol or diabetes. Lacunar strokes, a subtype, happen in tiny vessels deep in the brain and are strongly linked to long-term high blood pressure. These can sometimes cause milder symptoms, like slight weakness in one hand or slurred speech, which people might ignore.
Then there’s cryptogenic stroke-about 30% of ischemic cases-where doctors can’t find a clear cause after testing. These are the trickiest. They often point to hidden heart problems, like atrial fibrillation (AFib), where the heart beats irregularly and lets clots form.
Symptoms usually build over minutes to hours. Someone might wake up with a drooping face, or slowly lose the ability to speak clearly. The key sign? It’s gradual. That’s why people delay calling 999-they think it’s just a bad headache or fatigue.
Hemorrhagic Stroke: The Burst Vessel
Only about 13-15% of strokes are hemorrhagic, but they’re more deadly. Instead of a blockage, a blood vessel bursts inside or around the brain. This floods brain tissue with blood, crushing cells and increasing pressure.
There are two kinds: intracerebral hemorrhage (bleeding inside the brain tissue) and subarachnoid hemorrhage (bleeding on the brain’s surface). The latter is often caused by a ruptured aneurysm-a weak spot in a blood vessel that balloons like a bubble and pops.
What makes hemorrhagic strokes stand out? The symptoms hit like a lightning strike. A sudden, unbearable headache-described as "the worst headache of my life"-is the hallmark. So is vomiting, confusion, seizures, or losing consciousness right away. Eye problems like dilated pupils or gaze issues are also common. These aren’t subtle. They scream for emergency help.
High blood pressure is the biggest culprit. Around 80% of intracerebral hemorrhages happen because decades of uncontrolled hypertension have weakened small brain arteries. Even if you’ve never had a stroke before, if your blood pressure is above 140/90, you’re at risk.
How Do You Tell Them Apart?
On the outside, both types can look similar: weakness on one side, trouble speaking, dizziness. But the speed and intensity of symptoms give clues. Ischemic strokes creep in. Hemorrhagic ones explode.
Doctors rely on imaging-usually a CT scan-to know for sure. A CT can show bleeding instantly. For ischemic strokes, it might look normal at first, which is why follow-up MRIs are sometimes needed.
There’s new hope on the horizon. Blood tests for a protein called GFAP can now distinguish hemorrhagic from ischemic strokes within 15 minutes of a blood draw, with 92% accuracy. That could mean faster treatment in ambulances or even at home in the future.

Treatment: Fast, But Different
Time is brain-but the clock ticks differently depending on the stroke type.
For ischemic strokes, the goal is to dissolve or remove the clot. The gold standard is tPA (alteplase), a clot-busting drug given within 4.5 hours of symptom onset. A newer option, tenecteplase, works just as well and is easier to administer. If the clot is in a large artery, a mechanical thrombectomy-where a device physically pulls the clot out-can be done up to 24 hours after symptoms start, if imaging shows salvageable brain tissue.
Hemorrhagic strokes don’t respond to clot-busters. In fact, giving tPA to someone with bleeding in the brain can be deadly. Treatment here is about stopping the bleed and reducing pressure. That might mean surgery to clip an aneurysm, coil it from inside the artery, or drain excess blood. Medications to lower blood pressure fast are critical too.
Studies show that patients who reach a certified stroke center within 60 minutes have 15% better outcomes. That’s why every second counts-and why learning FAST (Face, Arm, Speech, Time) is so vital.
Prevention: Tailored to the Type
Preventing a stroke isn’t one-size-fits-all. You need a plan based on your risk type.
For ischemic stroke prevention:
- If you have atrial fibrillation, anticoagulants like apixaban or rivaroxaban cut stroke risk by 60-70%. Don’t skip doses.
- Aspirin (81mg daily) or clopidogrel helps prevent recurrence after a first stroke.
- Manage cholesterol with statins. Lowering LDL below 70 mg/dL reduces plaque buildup.
- Control diabetes. High blood sugar damages blood vessels over time.
For hemorrhagic stroke prevention:
- Keep your blood pressure under 120/80. The SPRINT trial showed this cuts hemorrhagic stroke risk by 38%.
- Avoid heavy alcohol and cocaine. Both spike blood pressure dangerously.
- Get screened for brain aneurysms if you have a family history or connective tissue disorders.
- Don’t smoke. Smoking weakens artery walls and raises blood pressure.
Both types benefit from:
- The Mediterranean diet-rich in olive oil, fish, nuts, vegetables. The PREDIMED study showed a 30% lower stroke risk.
- 150 minutes of brisk walking or cycling per week. That’s 30 minutes, five days a week.
- Weight management. Losing just 5-10% of body weight can drop blood pressure significantly.
What Happens After a Stroke?
Recovery depends on how much brain tissue was damaged and how fast treatment started. Many people regain function with rehab-physical therapy, speech therapy, occupational therapy.
But the real challenge is preventing a second stroke. Half of all strokes happen to people who’ve already had one. That’s why follow-up care is non-negotiable. Regular check-ups, medication adherence, and lifestyle changes aren’t optional-they’re survival tools.
One study found that patients who stuck to their blood pressure meds and attended rehab had 70% fewer repeat strokes over five years.

Why So Many Strokes Are Missed
One in four strokes is misdiagnosed-especially in younger adults or those with atypical symptoms. A woman might get sent home with "migraine" when she’s having a stroke. A young athlete might be told they’re "just tired."
That’s why everyone needs to know the signs, not just doctors. If something feels off-even if it’s mild or comes and goes-call 999. Don’t wait. Don’t drive yourself. Ambulances can start treatment on the way to the hospital.
The Bigger Picture
Stroke costs the UK and US billions each year in care, lost productivity, and long-term support. But the tide is turning. Telestroke networks now connect rural hospitals with neurologists in minutes. AI tools like Viz.ai help flag strokes on CT scans before a radiologist even sees them.
And prevention is working. Stroke death rates have dropped 25% in the last decade, mostly because more people are managing blood pressure and quitting smoking. But we’re not done. With an aging population, stroke cases will rise. The only way to beat it is to act early, act smart, and act together.
Final Thought: You Can’t Prevent Every Stroke, But You Can Prevent Most
Most strokes aren’t random. They’re the result of slow, silent damage-high blood pressure, smoking, inactivity, poor diet. You don’t need a miracle. You need consistency. Take your meds. Walk every day. Eat real food. Check your blood pressure. Talk to your doctor about your heart rhythm.
Stroke doesn’t care how old you are or how healthy you think you are. But your choices? They matter more than you know.
What’s the main difference between ischemic and hemorrhagic stroke?
Ischemic stroke is caused by a blood clot blocking an artery to the brain, while hemorrhagic stroke happens when a blood vessel bursts and bleeds into or around the brain. Ischemic strokes are more common (87%), but hemorrhagic strokes are often more severe and deadly.
Can you have a stroke and not know it?
Yes. Silent strokes happen without obvious symptoms, often detected only on brain scans. They still damage brain tissue and increase the risk of a major stroke or dementia later. High blood pressure and diabetes are major contributors.
Is aspirin safe for stroke prevention?
Aspirin can help prevent a second ischemic stroke by stopping clots, but it’s not for everyone. It can worsen bleeding in hemorrhagic stroke. Never take aspirin for stroke prevention without talking to your doctor first.
How quickly do you need to get help for a stroke?
For ischemic stroke, clot-busting drugs work best within 4.5 hours. Mechanical clot removal can work up to 24 hours if imaging shows salvageable brain tissue. For hemorrhagic stroke, every minute counts to control bleeding. Call 999 immediately-don’t wait to see if symptoms get better.
Can lifestyle changes really prevent stroke?
Absolutely. Controlling blood pressure, quitting smoking, eating a Mediterranean diet, and exercising 150 minutes a week can reduce stroke risk by up to 80%. Lifestyle isn’t just helpful-it’s the most powerful tool you have.

Jake Nunez
January 10, 2026 AT 07:08My uncle waited three hours because he thought it was a migraine. He's now in a nursing home. Don't be him.
Michael Marchio
January 12, 2026 AT 02:13lisa Bajram
January 13, 2026 AT 03:29Ted Conerly
January 13, 2026 AT 20:10Faith Edwards
January 14, 2026 AT 14:57Jay Amparo
January 14, 2026 AT 20:42Lisa Cozad
January 16, 2026 AT 16:36Saumya Roy Chaudhuri
January 16, 2026 AT 20:51anthony martinez
January 17, 2026 AT 00:50Mario Bros
January 17, 2026 AT 11:46Jaqueline santos bau
January 19, 2026 AT 01:28