Colitis Weight Management: Practical Guide to Maintaining a Healthy Weight
 Oct, 18 2025
Oct, 18 2025
Colitis Weight & BMI Calculator
Calculate Your BMI
Results & Guidance
Colitis Consideration: BMI is an important indicator, but during flare-ups, weight fluctuations may not reflect true nutritional status. Focus on symptom management and consult your healthcare provider for personalized guidance.
Living with Colitis is a daily balancing act. One of the trickiest parts is keeping your weight in a healthy range when flare‑ups can sap appetite or force you to avoid whole food groups. This guide walks you through proven strategies-diet tweaks, smart exercise, hydration habits, and stress‑busting routines-that help you stay on target without triggering symptoms.
Key Takeaways
- Track your Body Mass Index (BMI) to know where you stand.
- Choose a low‑residue or tailored anti‑inflammatory diet that respects your gut.
- Incorporate gentle, regular movement that supports digestion.
- Stay hydrated and consider supplementing with probiotics or targeted nutrients.
- Manage stress with proven mind‑body techniques to reduce flare‑ups.
Understanding the Weight Challenge in Colitis
Weight fluctuations in colitis are driven by three main forces: reduced nutrient absorption during active inflammation, altered appetite from pain or medication, and the body’s response to chronic stress. When you’re in remission, the goal shifts from merely avoiding weight loss to preventing excess gain-especially because obesity can worsen inflammation.
Step 1: Measure and Monitor Your Baseline
Start with a clear picture of where you are:
- Weigh yourself at the same time each morning, after using the bathroom.
- Calculate your BMI (weight kg ÷ height m²). A healthy range is 18.5‑24.9; aim for the middle of that band.
- Jot down any recent flare‑ups, medication changes, and bowel pattern logs. This data helps you spot trends.
Tracking tools like a simple spreadsheet or a phone app designed for IBD make it easier to see how diet, activity, and stress correlate with weight changes.
Step 2: Choose a Gut‑Friendly Eating Plan
The right diet supplies enough calories and nutrients while keeping the colon calm. Below is a quick comparison of three popular approaches for colitis patients.
| Strategy | Typical Foods | Fiber Level | Pros | Cons |
|---|---|---|---|---|
| Low‑Residue | White rice, peeled potatoes, well‑cooked carrots, tofu | Low | Minimizes stool bulk, reduces urgency during flare‑ups | May lack some nutrients; need supplementation |
| High‑Fiber (when in remission) | Oats, berries, legumes, whole‑grain bread | High | Supports gut microbiome, helps maintain healthy weight | Can trigger symptoms if inflammation returns |
| Mediterranean (anti‑inflammatory) | Olive oil, fish, nuts, leafy greens, tomatoes | Moderate | Rich in omega‑3s, antioxidants; promotes overall heart health | Requires careful portion control to meet calorie needs |
During active flare‑ups, most clinicians recommend the low‑residue approach because it limits the amount of undigested material reaching the colon. When you’re in remission, you can gradually re‑introduce higher‑fiber foods to boost nutrient density and support a healthy gut microbiome.
Step 3: Build Meals Around Nutrient Density
Even on a low‑residue plan, you can keep calories up:
- Protein: Soft‑cooked eggs, salmon, cottage cheese, tofu. Aim for 1.2‑1.5 g per kilogram of body weight.
- Healthy Fats: Avocado, olive oil, nut butter (smooth). Fats are calorie‑dense and gentle on the gut.
- Carbohydrates: White rice, mashed potatoes, ripe bananas, well‑cooked squash.
- Micronutrients: A multivitamin covering vitamins D, B12, iron, and calcium helps offset any gaps.
Use the Probiotics that are proven to survive stomach acid-such as Lactobacillus rhamnosus GG or Saccharomyces boulardii. Studies show they can reduce the severity of flare‑ups and improve nutrient absorption, which indirectly supports weight stability.
Step 4: Gentle Exercise that Supports Digestion
Exercise isn’t just about burning calories; it helps regulate bowel motility and reduces stress. Pick activities that won’t jostle your abdomen too much:
- Walking (30 min, moderate pace) - easy on the gut, promotes blood flow.
- Yoga or Pilates-focus on core‑strength moves that encourage gentle abdominal massage.
- Low‑impact cycling or swimming-great for cardiovascular health without impact.
Aim for at least 150 minutes of moderate activity per week. If you’re in a flare‑up, scale back to short 10‑minute walks and listen to your body’s signals.
Step 5: Hydration and Electrolyte Balance
Diarrhea and medication side‑effects can deplete fluids quickly. Drink 2‑3 liters of water daily, and add an electrolyte solution if you’re losing more than a liter a day. Herbal teas like ginger or peppermint can also soothe the gut while adding fluid.
Step 6: Manage Stress to Prevent Weight Swings
Stress hormones (cortisol) can trigger inflammation and increase appetite, leading to weight gain. Integrate one or more of these practices:
- Mindfulness meditation-5‑10 minutes in the morning.
- Deep‑breathing exercises before meals to promote better digestion.
- Regular sleep schedule-7‑9 hours a night reduces cortisol spikes.
Keeping a journal of stress triggers linked to flare‑ups can help you adjust lifestyle factors before they affect weight.
Step 7: When to Seek Professional Guidance
If your weight drifts more than 5 % in either direction over a month, book an appointment with a dietitian who specializes in IBD. They can fine‑tune calorie goals, recommend medical nutrition therapy, and adjust supplement regimens.

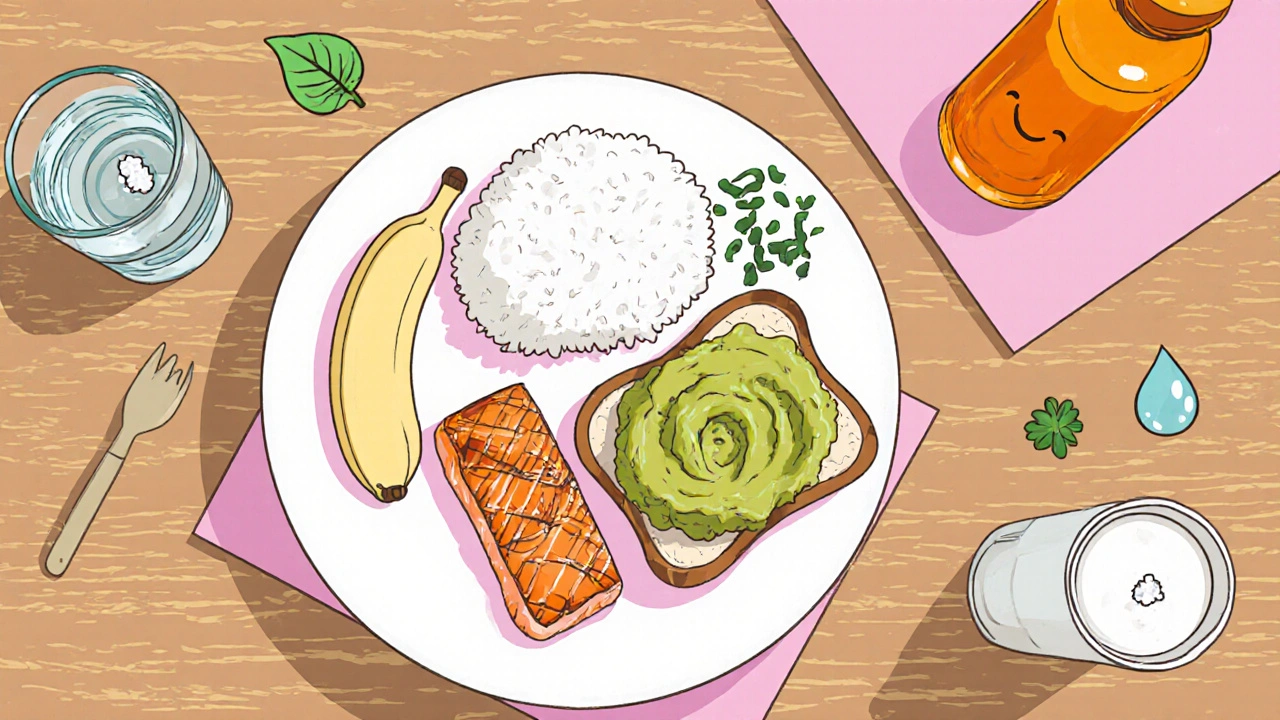
Putting It All Together: A Sample Day
Here’s a practical snapshot of a day that respects a low‑residue plan while keeping calories adequate:
- Breakfast: Scrambled eggs with a drizzle of olive oil, a side of peeled banana, and a small cup of probiotic‑rich kefir.
- Mid‑morning snack: Smooth avocado toast on white bread, plus a glass of water with a pinch of sea salt.
- Lunch: Grilled salmon, mashed potatoes, well‑cooked carrots, and a drizzle of lemon‑infused olive oil.
- Afternoon walk: 20‑minute brisk walk, followed by a few minutes of deep breathing.
- Snack: Greek yogurt (plain) blended with ripe peach puree.
- Dinner: Soft tofu stir‑fry with zucchini, peeled cucumber, and a side of white rice.
- Evening routine: 10‑minute guided meditation, a cup of ginger tea, and a multivitamin.
This routine provides roughly 2,200 kcal, 70 g protein, and enough healthy fats to keep you full without stressing the colon.
Common Pitfalls and How to Avoid Them
- Skipping meals: It may seem easier during flare‑ups, but it reduces calorie intake and can worsen weight loss.
- Relying on junk food: Processed carbs cause rapid spikes in blood sugar and can aggravate inflammation.
- Over‑exercising: Intense cardio can trigger gastrointestinal distress; stick to moderate, consistent activity.
- Neglecting supplements: Vitamin D, B12, and iron deficiencies are common in colitis; a daily regimen is vital.
Quick Reference Checklist
- Measure weight and BMI weekly.
- Follow a low‑residue diet during flare‑ups; transition to higher‑fiber foods in remission.
- Include protein‑rich foods at every meal.
- Drink at least 2 L of water daily; add electrolytes if needed.
- Exercise 150 min per week, focusing on low‑impact activities.
- Practice daily stress‑reduction techniques.
- Consult an IBD‑trained dietitian if weight shifts >5 %.
Frequently Asked Questions
Can I lose weight safely if I’m stuck in a flare‑up?
Yes, but it requires a calorie‑dense, low‑residue diet and regular monitoring. Focus on protein and healthy fats, stay hydrated, and avoid high‑fiber foods that can worsen diarrhea.
Is the Mediterranean diet safe for colitis patients?
During remission, the Mediterranean diet’s moderate fiber and anti‑inflammatory fats can be beneficial. During active inflammation, stick to low‑residue options and gradually re‑introduce Mediterranean components as symptoms improve.
How many calories should I aim for each day?
A good starting point is 30‑35 kcal per kilogram of body weight, adjusted up if you’re losing weight quickly or down if you’re gaining too much. For a 70 kg adult, that’s roughly 2,100‑2,450 kcal.
Do probiotics really help with weight management?
Research shows specific strains (e.g., Lactobacillus rhamnosus GG, Saccharomyces boulardii) can reduce inflammation, improve nutrient absorption, and modestly aid weight stability in IBD patients.
What’s the best way to track my progress?
Combine weekly weight/BMI checks with a food and symptom journal. Many apps let you log meals, pain scores, and bowel movements-all in one view to spot patterns.

Poornima Ganesan
October 18, 2025 AT 14:16First and foremost, if you’re not logging your weight and BMI every morning, you’re basically flying blind, and that’s unacceptable for anyone who claims to manage colitis intelligently. The guide correctly highlights the need for a consistent weigh‑in, but it glosses over the fact that people with fluctuating bowel habits should also track their fluid balance hourly. A low‑residue diet can be nutritionally sparse, so supplementing with a multivitamin isn’t optional-it’s mandatory. Moreover, the recommended 1.2–1.5 g protein per kilogram should be calculated with precision; otherwise you risk muscle loss during a flare. Finally, remember that stress‑reduction isn’t a nice‑to‑have, it’s a clinical necessity, so schedule mindfulness sessions like you would a medication dose.
By treating these metrics as non‑negotiable, you’ll avoid the common pitfall of “just winging it” and keep your weight stable even when inflammation spikes.
Brian Van Horne
October 26, 2025 AT 15:46While the guide offers a comprehensive overview, it could benefit from a succinct executive summary that distills the core recommendations into a single, actionable checklist. Such an approach would serve both clinicians and patients seeking rapid reference.
Norman Adams
November 3, 2025 AT 04:25Oh great, another “miracle” diet that works only if you ignore basic human biology.
Margaret pope
November 10, 2025 AT 03:05Look you can actually keep your weight on track without turning every meal into a science experiment just stay consistent with your weigh‑ins and make sure you’re getting enough protein and healthy fats it’s not that hard keep a simple log and you’ll see patterns emerge
Linda A
November 16, 2025 AT 11:51The body, in its quiet rebellion, often whispers truths about balance long before the mind can articulate them. In the context of colitis, weight becomes a metric of that dialogue, not merely a number to chase. By honoring the subtle cues of hunger and fatigue, you align with a deeper rhythm that surpasses any diet plan. Thus, the guide’s emphasis on mindfulness is, in essence, a call to listen to that inner philosopher.
Alex Lineses
November 22, 2025 AT 06:45Implementing a robust weight‑management protocol in colitis hinges on integrating multidisciplinary data streams, including anthropometric measurements, nutrient density matrices, and autonomic stress indices.
First, establish a baseline BMI within the optimal 18.5–24.9 window and record it in a digital health journal synchronized with your electronic medical record.
Second, calibrate caloric intake using the Harris‑Benedict equation adjusted for disease activity factor, ensuring a surplus of 250–500 kcal during remission phases to counteract malabsorption.
Third, prioritize protein synthesis pathways by targeting 1.3–1.5 g kg⁻¹ body weight of high‑bioavailability sources such as whey isolate, gall‑bladder‑friendly fish, and tempeh, thereby mitigating sarcopenia risk.
Fourth, embed omega‑3 enriched phospholipids into each meal, as eicosapentaenoic acid (EPA) modulates the NF‑κB cascade, attenuating systemic inflammation.
Fifth, employ low‑residue carbohydrate platforms-white rice, peeled starchy vegetables, and ripe bananas-to sustain glycogen stores without overloading colonic fermentative capacity.
Sixth, supplement with a comprehensive micronutrient pack covering vitamin D, B12, iron, and zinc, as deficiencies correlate with disease exacerbation and weight instability.
Seventh, integrate a structured aerobic regimen of 150 minutes per week, emphasizing low‑impact modalities such as brisk walking, aquatic therapy, or elliptical training to preserve joint integrity while enhancing gut motility.
Eighth, complement aerobic work with bi‑weekly resistance sessions targeting major muscle groups, thereby stimulating mTOR pathways and promoting lean mass accretion.
Ninth, maintain hydration at a minimum of 2.5 L/day, augmenting with isotonic electrolyte solutions during flare‑ups to counteract diarrheal losses.
Tenth, monitor cortisol fluctuations via salivary assays before and after stress‑reduction interventions, adjusting mindfulness practices accordingly.
Eleventh, adopt a stepped mindfulness protocol-beginning with diaphragmatic breathing, progressing to body‑scan meditation, and culminating in guided visualization-to systematically downregulate HPA‑axis activity.
Twelfth, conduct weekly reflective journaling that cross‑references symptom scores, dietary intake, and exercise metrics, enabling pattern recognition and predictive analytics.
Thirteenth, schedule quarterly consultations with an IBD‑specialized dietitian to recalibrate macro‑ and micronutrient prescriptions based on evolving clinical status.
Fourteenth, leverage telehealth platforms for real‑time data sharing with your gastroenterology team, fostering proactive intervention.
Fifteenth, remain vigilant for medication‑induced metabolic side effects, adjusting therapeutic regimens in collaboration with your prescriber.
Finally, cultivate a community support network-online forums, local meet‑ups, or peer‑coaching groups-to sustain motivation and share empirically validated strategies, thereby transforming weight management from an isolated ordeal into a collaborative, data‑driven journey.
Emma Williams
November 27, 2025 AT 11:45I love how the guide pulls everything together it feels like a friendly checklist that anyone can follow
Stephanie Zaragoza
December 2, 2025 AT 02:51While the article is thorough, it unfortunately overlooks a critical nuance, namely the individual variability in fiber tolerance, which can dramatically alter patient outcomes, and this omission could mislead readers who are seeking a one‑size‑fits‑all solution.
James Mali
December 6, 2025 AT 04:05Honestly the guide feels like a rehash of old advice, nothing groundbreaking here.
Janet Morales
December 9, 2025 AT 15:25Seriously? You think sipping ginger tea is going to keep the weight steady while you’re battling chronic inflammation? That’s romanticizing the struggle, and it does a disservice to anyone actually trying to live with colitis.
Tracy O'Keeffe
December 12, 2025 AT 12:51Oh dear, another so called “miracle” plan that pretends to be scientific while actually just a hodgepodge of buzzwordy nonsense, it definatly sounds like a recipe for disappointment, not empowerment.
Rajesh Singh
December 14, 2025 AT 20:25From an ethical standpoint, advocating a calorie‑dense low‑residue diet without emphasizing the importance of equitable access to quality protein sources borders on irresponsibility, especially for patients in low‑income regions where food insecurity is a daily reality.