Generalized Anxiety Disorder: SSRIs, Benzodiazepines, and CBT Explained
 Nov, 29 2025
Nov, 29 2025
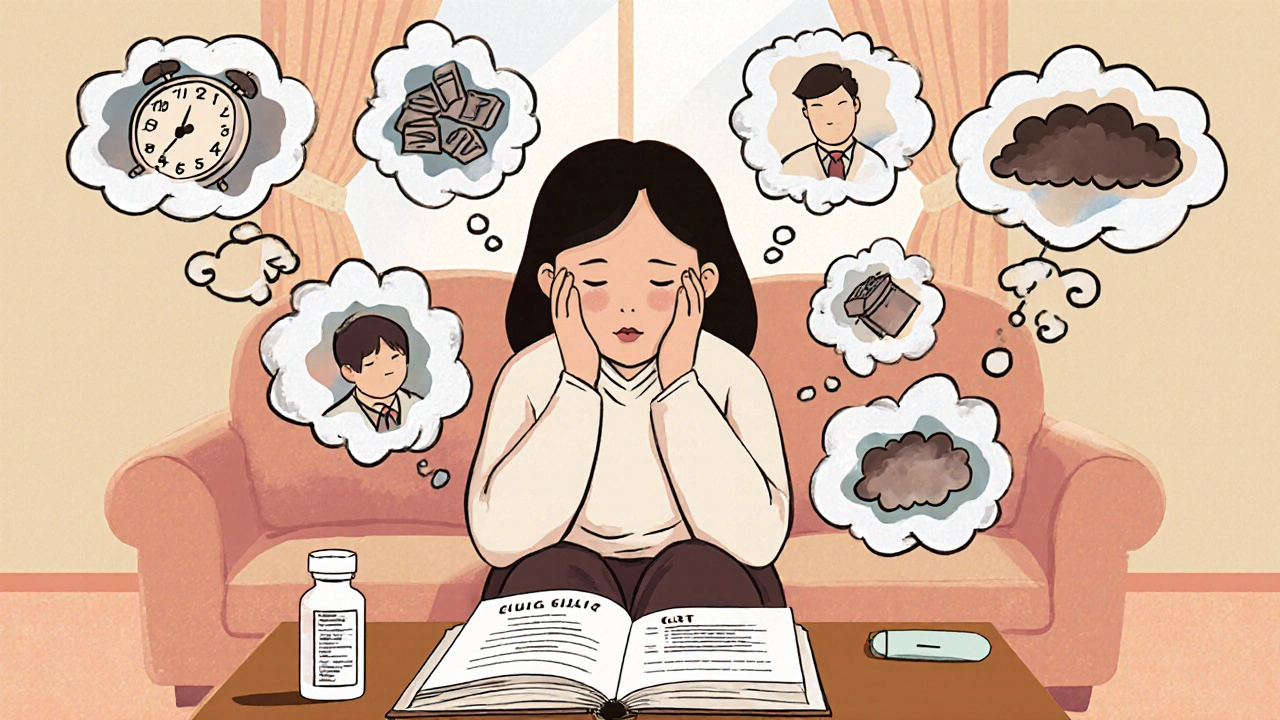
When you’re constantly worried-about work, health, money, even things that haven’t happened yet-it’s not just stress. It’s generalized anxiety disorder (GAD). The DSM-5 defines it as excessive worry on most days for at least six months, paired with symptoms like restlessness, fatigue, trouble concentrating, irritability, muscle tension, or sleep problems. It’s not something you can just "snap out of." And if you’ve been struggling with this, you’re not alone. About 6.8 million American adults live with GAD each year, and women are twice as likely to be affected as men.
Why SSRIs Are the First-Line Treatment
Selective serotonin reuptake inhibitors, or SSRIs, are now the go-to medication for GAD. Drugs like escitalopram (Lexapro), sertraline (Zoloft), and paroxetine (Paxil) work by increasing serotonin levels in the brain. But they don’t work overnight. It takes 2 to 6 weeks before you start feeling better. That’s why many people quit too soon, thinking the medication isn’t working.Here’s what the data shows: in clinical trials, about 50-60% of people with GAD respond to SSRIs. That’s not perfect, but it’s better than placebo. And unlike benzodiazepines, SSRIs don’t cause dependence. They’re safe for long-term use. The American Psychiatric Association and NICE guidelines both list SSRIs as first-line treatment for a reason.
Side effects? Yes. Nausea, especially in the first couple of weeks. Sexual dysfunction affects nearly half of users. That’s a big reason why some people stop taking them. But these side effects usually fade over time. Doctors often start with a low dose-like 25mg of sertraline-and slowly increase it to reduce early discomfort. If one SSRI doesn’t work, another might. There are several options, and finding the right one is part of the process.
The Fast Fix That Comes With a Cost
Benzodiazepines-like alprazolam (Xanax), lorazepam (Ativan), and diazepam (Valium)-work fast. Really fast. In 30 to 60 minutes, they calm the nervous system by boosting GABA, the brain’s main calming neurotransmitter. For someone in the middle of a panic attack or a crisis, that’s life-changing.But here’s the catch: they’re not meant for long-term use. After just a few months, your brain adapts. You need more to get the same effect. That’s tolerance. And when you try to stop? Withdrawal can be worse than the original anxiety-insomnia, tremors, rebound anxiety, even seizures in severe cases.
Studies show 40-50% of people on long-term benzodiazepines need higher doses within six months. The CDC and FDA now warn about abuse and dependence. Many insurance plans require prior authorization just to fill a prescription. And while they’re still used, they’re no longer first-line. They’re a bridge-not a destination.
Doctors still prescribe them, but carefully: short-term, low dose, with frequent check-ins. They’re best for acute flare-ups, not daily management. If you’ve been on them for more than 3 months, talk to your doctor about tapering. The Ashton Manual offers a proven, slow tapering schedule that can take 8 to 16 weeks. Don’t quit cold turkey.
CBT: The Skill-Based Solution
Cognitive Behavioral Therapy, or CBT, is the other first-line treatment for GAD. It doesn’t involve pills. It involves learning. Over 12 to 20 weekly sessions, you work with a therapist to identify anxious thoughts, challenge them, and change how you respond.For example, if you think, "If I make a mistake at work, I’ll get fired and end up homeless," CBT helps you ask: "What’s the evidence? What’s the worst that could actually happen? What’s a more realistic outcome?" Then you practice facing worries directly-like writing down your fears and sitting with them without reacting. That’s called worry exposure.
Studies show CBT is just as effective as SSRIs after 12 weeks. But here’s the kicker: at the one-year mark, people who did CBT are less likely to relapse. Only 25% return to high anxiety levels, compared to 45% after stopping medication. Why? Because CBT gives you tools. You don’t need a prescription to use them.
But it’s not easy. Homework is required. You have to practice skills between sessions. Only about 65-75% of people stick with it. The initial sessions can feel uncomfortable-you’re confronting fears head-on. But 87% of patients on platforms like Psychology Today report "good" or "excellent" outcomes.
The biggest barrier? Cost and access. A single session can cost $100-$150. Not all therapists are trained in CBT. There are only about 0.5 certified CBT therapists per 10,000 adults with anxiety in the U.S. But digital options are helping. Apps like Woebot and SilverCloud are FDA-cleared and have shown real results in clinical trials.

What Works Best? Combining Them
You don’t have to choose just one. The most effective approach for many people is combining SSRIs and CBT. A 2022 JAMA Network Open study found that 65% of patients using both reached remission, compared to 48% with just one treatment.Why does this work? SSRIs reduce the physical intensity of anxiety-making it easier to sit with discomfort during CBT. CBT, in turn, helps you stay off medication long-term by building resilience. It’s not about replacing one thing with another. It’s about layering support.
Even the VA/DoD guidelines now recommend this combo for patients who don’t fully respond to one treatment alone. And with the rise of telehealth, it’s easier than ever to get both a psychiatrist for medication and a therapist for CBT-all from home.
What’s New in 2025?
The field is evolving. In 2023, the FDA approved zuranolone (Zurzuvae), a new drug that works on GABA receptors like benzodiazepines-but with far less risk of dependence. In trials, only 5% of users had withdrawal symptoms, compared to 25% with traditional benzos.Genetic testing is also becoming available. Companies like GeneSight analyze your CYP2C19 and CYP2D6 genes to predict how you’ll metabolize SSRIs. If you’re a slow metabolizer, you might get side effects from standard doses. This can cut trial-and-error time in half.
Digital CBT platforms are booming. Headspace and Calm have millions of users. While they’re not replacements for therapy, they’re great for maintenance, relapse prevention, and filling gaps in care. The 2022 Mental Health Access Improvement Act also expanded Medicare coverage for licensed counselors, making CBT more affordable.

What Should You Do?
If you’re newly diagnosed with GAD, here’s a realistic path:- Start with an SSRI. Give it 6 weeks. Don’t quit early.
- Pair it with CBT. Even 8 sessions can make a difference.
- Avoid benzodiazepines unless you’re in crisis. And if you’re already on them, don’t stop abruptly-work with your doctor on a taper.
- Use apps like Woebot or Calm to reinforce skills between sessions.
- Track your progress. Note when anxiety spikes and what helped.
There’s no magic bullet. But there are proven paths. SSRIs help you feel calmer. CBT helps you stay calm. Benzodiazepines? They’re a temporary shield-not a sword.
The goal isn’t to eliminate anxiety entirely. It’s to stop letting it run your life. And with the right tools, you can do that.
Can I take benzodiazepines and SSRIs together?
Yes, but only under close medical supervision. Doctors sometimes combine them short-term-for example, using a benzodiazepine while waiting for an SSRI to kick in. But long-term use together increases sedation, fall risk, and cognitive impairment. It’s not a routine strategy and should only happen if other options have failed.
How long does it take for SSRIs to work for anxiety?
Most people start noticing improvements in 2 to 4 weeks, but full effects usually take 6 to 8 weeks. It’s common to feel worse before you feel better due to initial side effects like nausea or jitteriness. Stick with it. If there’s no change after 8 weeks, talk to your doctor about switching or adding CBT.
Is CBT better than medication for anxiety?
CBT and SSRIs are equally effective in the short term. But CBT wins in the long run. People who complete CBT are less likely to relapse after treatment ends. Medication treats symptoms; CBT teaches you how to manage your thoughts and reactions. If you want lasting change, CBT is the stronger choice-especially if you can access it.
Can I stop SSRIs once I feel better?
Don’t stop abruptly. Even if you feel fine, stopping SSRIs too soon increases relapse risk. Most doctors recommend staying on them for at least 6 to 12 months after symptoms improve. For people with chronic GAD, longer-term use may be necessary. Always taper under medical supervision to avoid withdrawal symptoms like dizziness, brain zaps, or mood swings.
Are there natural alternatives to SSRIs and benzodiazepines?
Exercise, sleep hygiene, and mindfulness can help reduce anxiety symptoms-but they’re not replacements for evidence-based treatments like SSRIs or CBT. Supplements like magnesium or ashwagandha have weak evidence and aren’t regulated. If you’re considering them, talk to your doctor. They can interact with medications or mask worsening symptoms.
What Comes Next?
If you’re starting treatment, give yourself time. Progress isn’t linear. Some weeks will feel harder than others. That’s normal. The key is consistency-whether it’s taking your pill daily, showing up for therapy, or doing your CBT homework.If you’re struggling to afford care, look into community mental health centers, sliding-scale therapists, or digital CBT apps. Many employers offer EAPs (Employee Assistance Programs) with free counseling sessions.
And if you’ve tried everything and still feel stuck? You’re not broken. You just haven’t found the right combination yet. The science is clear: GAD is treatable. It just takes patience, the right tools, and support.

Erin Nemo
November 30, 2025 AT 21:52I started Lexapro last month and honestly? The first two weeks were hell-nausea, jittery, felt like my brain was buzzing. But now? I can breathe again. No magic, just time.
ariel nicholas
December 1, 2025 AT 19:29SSRIs? Please. Big Pharma’s latest scam to keep you docile and dependent. You think serotonin fixes anxiety? Nah-it’s your soul screaming for meaning in a capitalist hellscape. Stop swallowing pills and start asking: Why are you so anxious in the first place?
Rachel Stanton
December 3, 2025 AT 13:41Just want to add that CBT isn't just "thinking positive"-it's neuroplasticity in action. When you reframe catastrophic thoughts, you're literally rewiring your amygdala. And yes, it's hard. But the 25% relapse rate after CBT? That’s the power of skill-building over symptom suppression. If you can access even 8 sessions, it’s worth every minute.
Amber-Lynn Quinata
December 3, 2025 AT 17:07Why do people keep saying "just take SSRIs" like it’s a vitamin? 😒 I’ve been on Zoloft for 3 years and my sex drive is GONE. My therapist says "it’s worth it"-but who decided that? 😔 My husband doesn’t even kiss me anymore. This isn’t treatment-it’s emotional sacrifice.
Lauryn Smith
December 4, 2025 AT 09:30I was skeptical about CBT too. Thought it was just talking. But after 10 sessions, I caught myself thinking, "Wait, that’s not even realistic," and I laughed. That moment? That’s when I knew it was working. No pills. Just practice.
Bonnie Youn
December 4, 2025 AT 21:34STOP WAITING FOR THE MEDS TO WORK AND JUST DO CBT ALREADY!! I was stuck for 5 years on Xanax until I found a therapist who didn’t let me quit. Now I’m 2 years anxiety-free. You don’t need permission to get better-you need action. Go. Now. 💪
Edward Hyde
December 6, 2025 AT 03:33SSRIs make you feel like a zombie with a credit card. Benzodiazepines? That’s the real high. But yeah, I get it-doctors don’t wanna get sued. So they give you a placebo with a fancy name and call it "treatment." Meanwhile, I’m still up at 3 a.m. wondering if my cat hates me.
Charlotte Collins
December 7, 2025 AT 18:33It’s fascinating how the medical-industrial complex co-opts psychological distress into a pharmacological problem. CBT is framed as "empowering," but only if you can afford $120/hour. Meanwhile, the same system that profits from SSRIs also denies access to therapy. The irony is thick enough to spread on toast.
Margaret Stearns
December 9, 2025 AT 10:30Just wanted to say thank you for this post. I’ve been on sertraline for 9 months. Side effects faded. CBT helped me notice when I’m catastrophizing. I still have bad days. But now I know they’re just days-not the end of the world.
amit kuamr
December 10, 2025 AT 17:58SSRIs work only if you believe in them. In India we use yoga and chai. No pills needed. Your system is broken. You need to fix your mind not your chemistry
Scotia Corley
December 11, 2025 AT 00:04While the empirical data supporting SSRIs and CBT is robust, one must consider the epistemological limitations of randomized controlled trials in the context of phenomenological experience. Anxiety is not a biomarker-it is an existential condition. Reducing it to pharmacological or behavioral interventions risks ontological reductionism.
elizabeth muzichuk
December 12, 2025 AT 06:30I’m so mad at my doctor for putting me on Xanax for 8 months. I didn’t even know I was addicted until I tried to quit and had seizures. Now I’m in therapy and I feel like I’ve been gaslit my whole life. Why didn’t anyone tell me this was dangerous? 😭
Debbie Naquin
December 12, 2025 AT 22:45CBT doesn’t eliminate anxiety-it decouples it from identity. The thought isn’t you. The fear isn’t truth. The body’s alarm isn’t a prophecy. That’s the real shift. Not chemistry. Not coping. Recognition.
Karandeep Singh
December 13, 2025 AT 19:48Benzos are fine if you use them right. People panic and quit SSRIs too fast. I took Xanax for 2 weeks while waiting for Lexapro to kick in. Worked. No problem. Stop the drama