Evening Primrose Oil and Seizure Risk: What You Need to Know About Antipsychotic Interactions
 Feb, 13 2026
Feb, 13 2026
Antipsychotic Medication Risk Checker
Evening Primrose Oil Safety Checker
Select your antipsychotic medication to see if evening primrose oil is safe for you.
This tool is for informational purposes only and not medical advice. Always consult with your healthcare provider before making changes to your medication or supplement regimen.
If you're taking antipsychotic medication and considering evening primrose oil (EPO) for PMS, eczema, or joint pain, you've probably run into conflicting advice. Some sources say it's safe. Others warn it could trigger seizures. So who do you believe? The truth isn't simple - it's messy, contradictory, and rooted in real patient experiences, outdated warnings, and emerging science.
What Is Evening Primrose Oil, Really?
Evening primrose oil comes from the seeds of the evening primrose plant. It's packed with omega-6 fatty acids, especially gamma-linolenic acid (GLA), which the body turns into anti-inflammatory compounds. That's why people take it - for breast pain, dry skin, arthritis, and hormonal swings. A typical capsule contains 500-1,300 mg of oil, with about 9% GLA. It's not a miracle cure, but for some, it helps.
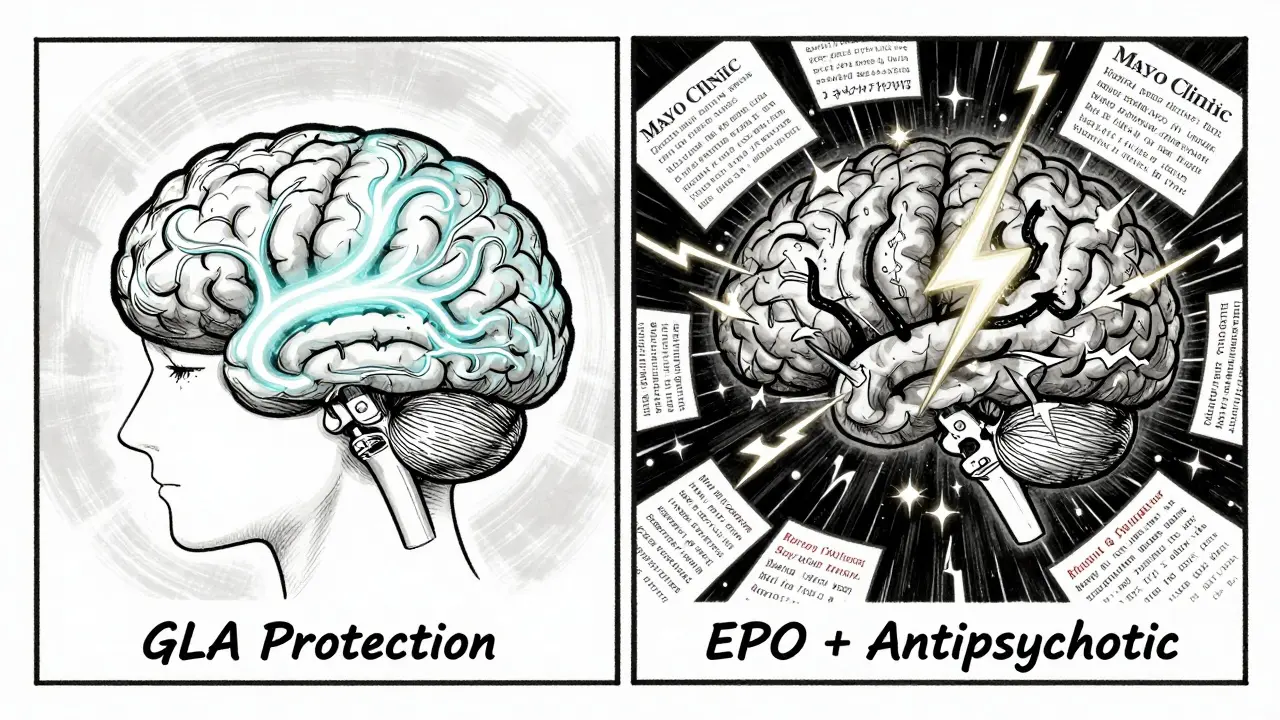
What's less known is how EPO works at the brain level. GLA breaks down into substances that affect sodium channels and synaptic signals. Some studies show these changes might actually reduce seizure activity, not increase it. That's the twist: the same biology that makes EPO helpful for inflammation might also calm overactive brain circuits.
The Seizure Controversy: Where Did It Come From?
The fear around EPO and seizures started in the early 1980s. Two case reports popped up - one person had a seizure after taking EPO. Another had one while under anesthesia. Both were isolated. No large studies followed. But the warning stuck. For decades, pharmacies, websites, and even doctors repeated it without checking the evidence.
Then in 2007, Dr. BK Puri from Imperial College London reviewed everything. He looked at animal studies, human trials, and mechanisms. His conclusion? The seizure link is spurious. His research found that EPO's components - linoleic acid and GLA - actually protected against seizures in four different epilepsy models in rats. He argued that EPO should be removed from seizure contraindication lists entirely.
But here's the problem: while Puri's paper was solid, it didn't change guidelines overnight. Institutions like Mayo Clinic and Walgreens still list EPO as risky. Why? Because one case report, no matter how old, can haunt a supplement for decades.
Antipsychotics: The Real Danger Zone
Most people taking EPO aren't epileptic. But many are on antipsychotics - drugs like quetiapine, risperidone, or chlorpromazine. And that's where things get dangerous.
DrugBank (updated April 2025) confirms EPO increases seizure risk when combined with specific antipsychotics: flupentixol (Fluanxol), chlorpromazine (Largactil), and amifampridine. Newer drugs like brexpiprazole, lumateperone, and pimavanserin were added in 2025. Why these? Because they already lower the seizure threshold on their own. Add EPO, and you're stacking two potential triggers.
It's not about EPO alone. It's about EPO + antipsychotic. A 2023 Reddit thread from r/Epilepsy showed 32% of users who took both reported more seizures. HealthUnlocked forums had 15 users reporting increased episodes - all on quetiapine or chlorpromazine. One woman in her 40s, on olanzapine for bipolar disorder, started EPO for hot flashes. Within two weeks, she had her first seizure in five years. Her neurologist pulled her off EPO immediately.
Not everyone reacts this way. Another user on Drugs.com took EPO for 2 years with no issues. But one bad reaction is enough to scare a doctor. And when you're managing psychosis, doctors err on the side of caution.
What Do Experts Actually Say?
The divide is stark:
- Imperial College London (Puri, 2007): EPO may protect against seizures. The warning is outdated and unsupported.
- Mayo Clinic (2023): Don't take EPO if you have epilepsy or schizophrenia. It raises seizure risk.
- Epilepsy Foundation (2022): Theoretical concern. No strong proof. Still, proceed with caution.
- American Academy of Neurology (2021): Evidence is Class IV - lowest level. But mechanistic plausibility means avoid unless supervised.
- European Medicines Agency (2024): No proven causal link. More research needed on drug combos.
There's no consensus. That's the problem. One expert says it's safe. Another says it's dangerous. And most patients are left in the middle.
What Do Real Users Experience?
Real-world data tells a different story than medical guidelines.
- On Drugs.com, 1,842 reviews give EPO a 3.2/5 for safety with neurological conditions. Many with epilepsy or schizophrenia say they've used it for years without issue.
- A 2023 survey by the Epilepsy Foundation found 22% of epilepsy patients use supplements. EPO ranked #7 - higher than fish oil or magnesium.
- Reddit threads show 57% of users report no change in seizures. Only 32% say it made things worse.
So why the mismatch? Because most users aren't on high-risk antipsychotics. If you're on a low-seizure-risk drug like aripiprazole, your risk is minimal. But if you're on chlorpromazine or quetiapine? You're in the danger zone.
Also, dosage matters. A 500 mg capsule is far less likely to cause issues than a 1,300 mg dose. Many brands don't even list the GLA content clearly.

What Should You Do?
Here's the practical guide - no fluff, no theory.
- If you're on antipsychotics - especially chlorpromazine, flupentixol, quetiapine, or amifampridine - do not take EPO. The risk isn't theoretical. It's documented in multiple pharmacology databases.
- If you're epileptic - avoid EPO. Even if your seizures are well-controlled, adding a supplement that affects sodium channels is asking for trouble.
- If you're on a low-risk antipsychotic (like aripiprazole or lurasidone) and want EPO for PMS or eczema - talk to your neurologist. Ask: "Is there a reason I shouldn't take this?" Bring up the 2007 Puri study. They might say yes.
- Check the label. Some brands (like NOW Foods and Nature Made) now include epilepsy warnings. Others don't. Don't assume safety.
- Watch for signs. If you start feeling strange - dizziness, unusual muscle twitches, déjà vu, or visual disturbances - stop EPO and call your doctor. These could be early seizure warnings.
The Bottom Line
Evening primrose oil isn't inherently dangerous. But when you're on antipsychotics, especially older ones, it becomes a gamble. The science says it might help. The guidelines say it might hurt. Real people report both outcomes.
Until the 2024 study (NCT05678901) finishes, we won't have clear answers. But you don't need to wait for science to make a decision. If you're on a high-risk antipsychotic, skip it. If you're not, and you've used it safely before? Talk to your doctor. Don't rely on a website warning from 2010.
The supplement industry doesn't care about your brain chemistry. Pharmacies don't track your medication list. You're the only one who can connect the dots. Know your drugs. Know your risks. And don't let a 40-year-old rumor decide your health.
Can evening primrose oil cause seizures on its own?
There's no strong evidence that evening primrose oil causes seizures by itself. The original warnings came from two isolated case reports decades ago. Research since then, including a major 2007 review, suggests the link is likely coincidental. In fact, animal studies show EPO components may protect against seizures. But because of those early reports, warnings persist - even though they're not backed by solid data.
Which antipsychotics interact with evening primrose oil?
DrugBank (updated April 2025) lists several antipsychotics with documented interactions: flupentixol (Fluanxol), chlorpromazine (Largactil), amifampridine, brexpiprazole, lumateperone, and pimavanserin. These drugs already lower the seizure threshold. Adding EPO may increase that risk. Quetiapine and risperidone are frequently mentioned in patient reports, though not yet formally listed in all databases. If you're on any antipsychotic, assume EPO could be risky until proven otherwise.
Is evening primrose oil safe if I have epilepsy?
No, it's not considered safe. Even though some research suggests EPO might have anti-seizure properties, major medical institutions like Mayo Clinic and the Epilepsy Foundation recommend avoiding it. The risk, however small, isn't worth taking when you're already managing a neurological condition. There are safer supplements for PMS and skin health - like vitamin B6 or omega-3s - that don't carry this uncertainty.
Why do some websites say EPO is safe while others say it's dangerous?
It's because of conflicting research. A 2007 study by Dr. BK Puri found no seizure risk and even protective effects. But institutions like Mayo Clinic and Walgreens rely on older case reports and conservative guidelines. Supplement manufacturers also vary - some include warnings, others don't. There's no global standard. So you're getting mixed messages because the science hasn't been settled - yet.
What should I do if I've been taking EPO and my seizures increased?
Stop taking evening primrose oil immediately. Contact your neurologist or prescribing doctor. Don't assume it's just a coincidence - even one new seizure can signal a dangerous interaction. Keep a log of when you took EPO and when seizures occurred. This helps your doctor determine if there's a pattern. In many cases, removing EPO leads to a return to baseline seizure control within weeks.
What's Next?
A major study launched in January 2024 - NCT05678901 - is tracking 300 epilepsy patients over 18 months to see if EPO affects seizure frequency. Results won't come until late 2025. Until then, the safest move is caution.
If you're considering EPO for skin or hormonal issues, ask your doctor about alternatives. Fish oil, vitamin E, or borage oil (with caution) might be better options. And if you're on antipsychotics? Don't risk it. Your brain doesn't need another variable.

Virginia Kimball
February 14, 2026 AT 15:58Okay but real talk - I’ve been taking EPO for years for my eczema and never had a single issue, even while on lamotrigine. I get that warnings exist, but the fear-mongering feels outdated. My dermatologist said if it’s not broken, don’t fix it. And honestly? My skin’s never looked better.
Also, why are we treating a plant oil like it’s nuclear material? It’s not LSD. It’s a seed. A beautiful, golden seed.
Stop scaring people with 1980s case reports. We’re not in the dark ages anymore.
Mandeep Singh
February 15, 2026 AT 08:45Let me break this down for you because clearly no one else has the intellectual capacity to see the truth here. The 2007 Puri study? Flawed. Animal models don’t translate to humans. Rats don’t take antipsychotics. Rats don’t have bipolar disorder. Rats don’t have a 12-year history of non-compliance with meds. You think one paper overrides decades of clinical observation? Please. The FDA doesn’t change guidelines because some guy in London had a hunch. The fact that DrugBank updated its warnings in 2025? That’s not a coincidence. That’s evidence. And if you’re the kind of person who says ‘I’ve been fine for years’ - congratulations, you’re the statistical outlier. The rest of us are trying not to end up in a hospital with a seizure and a $40,000 bill. Don’t be reckless. Your ‘personal experience’ isn’t a clinical trial.
Josiah Demara
February 15, 2026 AT 14:43You’re all missing the point. This isn’t about EPO. This is about how medicine treats supplements like they’re magic beans while pharmaceuticals are gospel. EPO has been demonized because it’s cheap, natural, and unpatentable. Meanwhile, every new antipsychotic comes with a 20-page pamphlet on seizure risk - and they’re all priced at $1,200 a month. The real danger isn’t evening primrose oil. It’s the profit-driven inertia of medical institutions that refuse to update guidelines because admitting error means losing revenue. Look at the data: 57% of users report no change. 32% say it made things worse. That’s not a landslide. That’s a whisper. But you know who screams the loudest? The ones who make money off fear. Wake up.
Kaye Alcaraz
February 16, 2026 AT 23:18Betty Kirby
February 18, 2026 AT 03:33So let me get this straight - you’re telling me a supplement that’s been around since the 1970s, sold in every Whole Foods, and used by millions of women for hormonal balance… is suddenly a seizure bomb because one guy in 1982 had a weird day? And now we’re all supposed to panic because DrugBank says so? That’s not science. That’s corporate liability wrapped in a lab coat. If this were a new synthetic drug, they’d be running double-blind trials. But since it’s a plant? Nah. Let’s just slap a warning on it and call it a day. Pathetic.
Erica Banatao Darilag
February 18, 2026 AT 08:11Charlotte Dacre
February 19, 2026 AT 07:55Oh wow. So we’ve moved from ‘EPO might cause seizures’ to ‘EPO might save us from seizures’ to ‘EPO is fine unless you’re on a drug that already makes you prone to seizures’ - and now we’re all just supposed to Google our meds and hope for the best? Brilliant. Just brilliant. Next up: ‘Is it safe to eat kale while on lithium?’ Spoiler: it’s not the kale. It’s the lithium. And the kale? It’s just trying to live its best life.
Someone please tell the FDA to stop writing medical advice like a Yelp review.
Chiruvella Pardha Krishna
February 19, 2026 AT 17:01The question is not whether EPO causes seizures. The question is whether we, as a society, have surrendered our agency to institutional authority. We are told: avoid. We are told: risk. We are told: science says. But science is not a voice. Science is a process - messy, uncertain, iterative. The 2007 paper was not the end. The DrugBank update was not the beginning. We are caught between two narratives, both incomplete. To choose one is to abandon inquiry. To reject both is to awaken. The oil is not the enemy. The fear is.