Global Biosimilar Markets: Europe vs United States
 Feb, 16 2026
Feb, 16 2026
When you hear the word "generic," you probably think of cheap pills that do the same thing as brand-name drugs. But biosimilars aren’t like that. They’re not copies of a chemical pill. They’re copies of living, complex biologic medicines - drugs made from living cells, often used to treat cancer, autoimmune diseases, and diabetes. And when it comes to how these drugs are approved and used, Europe and the United States are playing two completely different games - even though they’re trying to reach the same finish line.
What Exactly Is a Biosimilar?
A biosimilar isn’t a generic. Generics are chemically identical to their brand-name counterparts. Biosimilars are highly similar - but not identical - to a reference biologic drug. Think of it like two handcrafted wooden chairs. They look the same, feel the same, and serve the same purpose. But one was made by a different craftsman using slightly different tools. That’s biosimilars: same function, same safety, same effectiveness, but made with a different biological process.
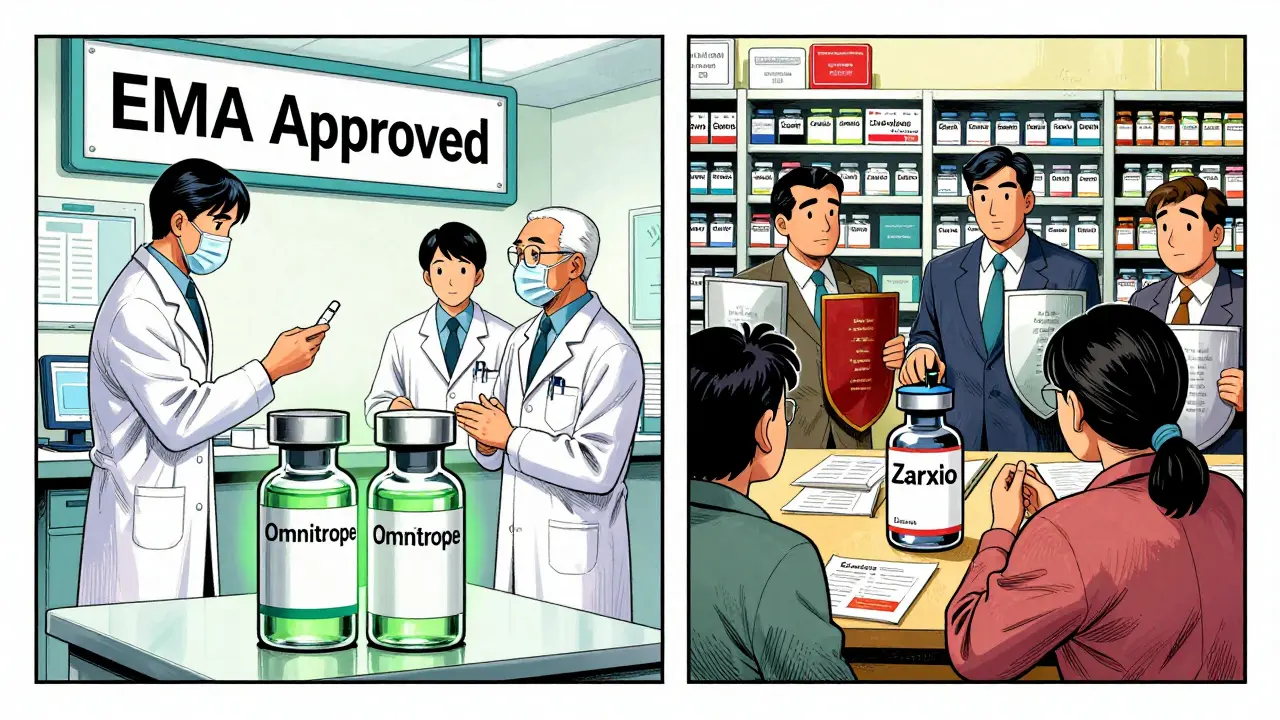
The first biosimilar ever approved was Omnitrope, a growth hormone, in Europe back in 2006. The European Medicines Agency (EMA) created the first clear rules for how to prove a biosimilar works. They didn’t demand a whole new set of clinical trials. Instead, they looked at the molecule’s structure, how it behaves in the lab, and a few targeted studies in patients. This "totality-of-evidence" approach saved time and money, and it worked. By 2024, Europe had approved over 100 biosimilars. The U.S. didn’t get its first until 2015 - Zarxio, a drug for low white blood cell counts. The delay wasn’t because the science was harder. It was because the system was slower.
Europe: The Pioneer with a Mature System
Europe didn’t just get there first. It built a system that made biosimilars easy to adopt. Hospitals in Germany, France, and the UK started using them almost as soon as they were approved. Why? Because the government and insurers pushed them. They ran tenders - competitive bidding - for drugs. If a biosimilar was 25% cheaper than the original, hospitals chose it. No debate. No paperwork. Just savings.
By 2024, Europe’s biosimilar market hit $13.16 billion in revenue, according to Precedence Research. That’s up from $8.9 billion in 2020. That’s a 13% annual growth rate. In some countries, biosimilars now make up over 80% of the market for drugs used to treat rheumatoid arthritis and Crohn’s disease. In oncology, they’re catching up fast. Sandoz, Fresenius Kabi, and Amgen dominate here. Germany, in particular, became a manufacturing hub. Companies from all over the world set up production there because the regulatory path was clear and the market was ready.
Doctors trust them. Patients accept them. Payers demand them. It’s a cycle: better regulation → faster adoption → lower prices → more use → more investment. Europe didn’t just allow biosimilars. It built an ecosystem around them.

United States: The Slow Starter, Now Accelerating
The U.S. had the same goal - lower drug costs - but the path was blocked. The Biologics Price Competition and Innovation Act (BPCIA) passed in 2009, but it came with a catch. It created a legal minefield called the "patent dance." Originator companies like AbbVie (maker of Humira) used every trick in the book: filing dozens of patents, dragging out lawsuits, and delaying biosimilar entry for years. Even when a biosimilar got FDA approval, it couldn’t hit the market for years because of legal battles.
By 2024, the U.S. had only approved 12 biosimilars - compared to over 100 in Europe. And many of those were for low-complexity drugs like filgrastim, used for infection prevention after chemotherapy. Complex drugs like Humira, Enbrel, and Remicade? Still mostly untouched by biosimilars.
But everything changed in 2024. The FDA dropped a bombshell: they no longer required switching studies to approve a biosimilar as "interchangeable." That meant a pharmacist could swap a biosimilar for the original drug without asking the doctor. In Europe, this had been standard for years. In the U.S., it was a huge barrier. Removing it was like taking down a toll booth on the highway to adoption.
Then came the Inflation Reduction Act of 2022. It eliminated the Medicare Part D coverage gap - the "donut hole" - and gave insurers a financial reason to push biosimilars. Why pay $10,000 for a biologic when a biosimilar costs $7,000 and the government helps cover the difference?
By 2024, the U.S. biosimilar market hit $10.9 billion. Projections show it could hit $30.2 billion by 2033. That’s an 18.5% annual growth rate - faster than Europe’s. Why? Because the U.S. has more high-value biologics coming off patent. Over 100 biologics will lose protection between 2025 and 2034. Humira alone represents a $232 billion opportunity. The market wasn’t slow because it didn’t want biosimilars. It was slow because the system was rigged. Now it’s unrigging.
Key Differences: Regulation, Adoption, and Price
Here’s the real contrast:
- Regulation: Europe’s EMA uses a streamlined, science-based process. The FDA used to demand extra clinical trials for interchangeability - now it doesn’t.
- Adoption: Europe’s centralized system means once a biosimilar is approved, it’s quickly added to hospital formularies. In the U.S., each hospital, insurer, and pharmacy decides independently - until now.
- Price: In Europe, biosimilars launch at 15-30% discounts. In the U.S., they’ve been priced higher - sometimes only 10% cheaper - because of patent delays and lack of competition. But with Humira biosimilars finally entering in 2023, prices are crashing. Some are now 70% cheaper than the original.
And here’s something surprising: Europe’s market is bigger today, but the U.S. is growing faster. North America (mostly the U.S.) is projected to overtake Europe in market size by 2027. Why? Because the U.S. has more money to spend on biologics. More patients. More high-cost drugs. More incentive to cut costs.

Who’s Winning?
It’s not a race with a winner. It’s two different paths to the same outcome: cheaper, effective drugs for millions.
Europe won the early game. They built the playbook. They proved biosimilars are safe. They showed doctors and patients it works. They created a culture of cost-conscious prescribing.
The U.S. is winning the next chapter. With Humira biosimilars now available, the dam has broken. Pfizer, Merck, and Samsung Bioepis are flooding the market. Insurers are pushing them. Patients are saving thousands. The FDA’s 2024 rule change is the turning point. The U.S. isn’t just catching up - it’s leapfrogging.
By 2030, biosimilars could save the U.S. healthcare system over $100 billion. In Europe, the savings are already in the tens of billions. Both markets are proving the same thing: when you make biosimilars easy to approve and easy to use, they don’t just compete - they transform.
What’s Next?
The future isn’t about Europe vs. the U.S. It’s about how fast biosimilars can reach patients. The next wave will be for even more complex drugs - like gene therapies and cell therapies. Manufacturing them is harder. Proving similarity is tougher. But the lessons from Europe and the U.S. are clear: regulation must be science-based, not legalistic. Payers must incentivize use. Doctors must be educated. Patients must be trusted.
The global biosimilars market is expected to hit $175 billion by 2034. That’s not just business. That’s better access. Lower costs. More treatment options. Whether it’s in a hospital in Berlin or a clinic in Chicago, the goal is the same: give patients the medicine they need without bankrupting them.
Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar versions of complex biologic drugs made from living cells - like Humira or Enbrel. Because biologics are made from living organisms, biosimilars can’t be identical - but they must have no clinically meaningful differences in safety or effectiveness.
Why did Europe adopt biosimilars faster than the U.S.?
Europe created a clear, science-driven regulatory path in 2006 and tied it to hospital procurement policies. Once approved, biosimilars were automatically included in tender systems, and doctors were educated on their safety. In the U.S., patent litigation, lack of interchangeability rules, and fragmented payer systems slowed adoption. The FDA’s 2024 rule change removing switching studies is now helping close the gap.
Can a pharmacist substitute a biosimilar for the original drug without a doctor’s approval?
In Europe, yes - for interchangeable biosimilars. In the U.S., only if the biosimilar is designated as "interchangeable" by the FDA. Before June 2024, this was nearly impossible to achieve. Now, with the FDA dropping the switching study requirement, more biosimilars are expected to gain interchangeable status, allowing pharmacists to substitute them automatically.
Which countries in Europe lead in biosimilar use?
Germany, France, and the United Kingdom lead in adoption. Germany also leads in manufacturing, with several major biosimilar producers based there. These countries use hospital tenders and mandatory substitution policies to drive uptake, especially in oncology and autoimmune disease treatments.
Why is the U.S. market growing so fast now?
Three big reasons: the FDA removed the switching study barrier for interchangeable status, the Inflation Reduction Act gave insurers financial incentives to use biosimilars, and major biologics like Humira finally lost patent protection. With 14 Humira biosimilars approved and prices dropping by up to 70%, adoption is accelerating faster than ever.

Kancharla Pavan
February 16, 2026 AT 15:58Let me be crystal clear-Europe didn't "win" anything. They just had the luxury of a single-payer system that could bully hospitals into submission. In the U.S., we have competition, innovation, and patient choice. You can't just force doctors to switch drugs because some bureaucrat in Brussels said so. Biosimilars are great in theory, but when you remove the incentive for R&D by crushing profits, you kill the pipeline. The next breakthrough cancer drug won't come from a government-mandated tender. It'll come from a venture-backed biotech in Boston or San Diego. Europe's model is a dead end disguised as efficiency.