Rosacea Facial Flushing and Topical Antibiotic Treatment: What Works and What Doesn’t
 Nov, 22 2025
Nov, 22 2025
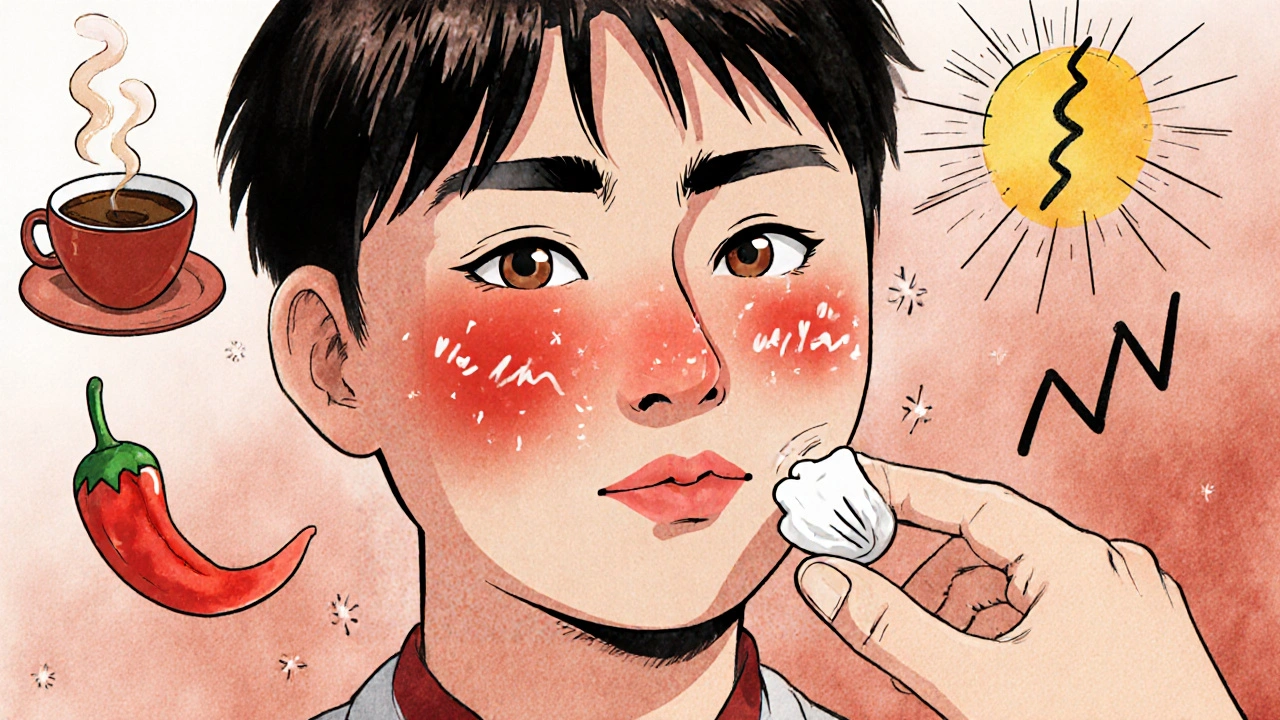
Facial flushing isn’t just blushing after a spicy meal or a stressful meeting. For millions of people, it’s the first sign of something deeper-rosacea. This chronic skin condition doesn’t go away on its own, and without the right treatment, it can get worse. The redness, bumps, and burning sensations don’t just affect your skin-they affect your confidence, your social life, even your mental health. And while there’s no cure, the right topical antibiotics can make a real difference. But not all treatments are created equal, and knowing what actually works-and what doesn’t-is key to managing this condition without frustration.
What Is Rosacea, Really?
Rosacea isn’t acne. It’s not just sensitive skin. It’s a persistent inflammatory condition that mainly hits the central face: cheeks, nose, chin, and forehead. The earliest and most common sign? Facial flushing. About 75% of people with rosacea experience this before anything else. It starts as a sudden warmth, a bright red glow, often triggered by heat, alcohol, stress, or even a hot cup of coffee. Unlike normal blushing, which fades in minutes, rosacea flushing can last for hours. And over time, that temporary redness becomes permanent.
That’s when the persistent redness sets in-what dermatologists call erythema. It’s not a sunburn you can wash off. It’s there all day, every day. Around 90% of rosacea patients develop this. Alongside it, you might see tiny visible blood vessels-telangiectasia-like fine red lines spreading across your cheeks. And then come the bumps: papules and pustules that look like acne but aren’t caused by oil or clogged pores. These are inflammatory lesions, and they’re where topical antibiotics come in.
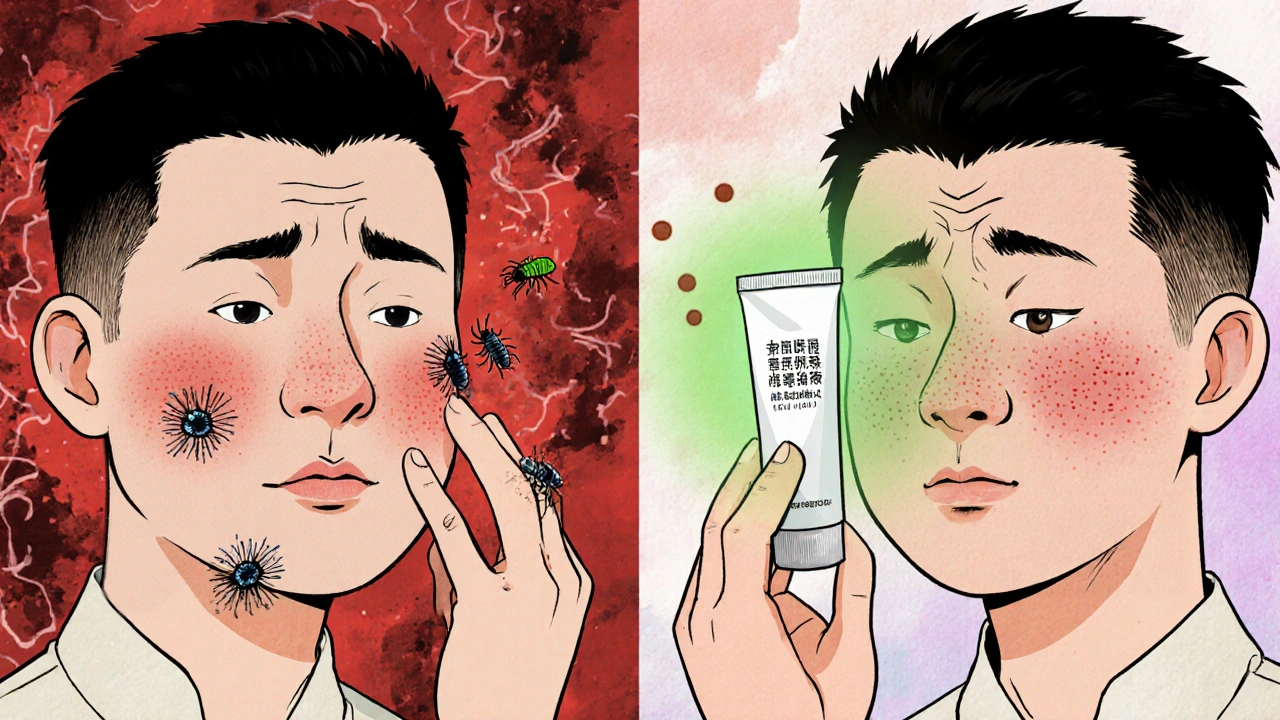
Why Topical Antibiotics? Not for Bacteria
You might think antibiotics are for infections. But in rosacea, they’re not fighting bacteria like acne does. Instead, they’re calming inflammation. The real culprits? Overactive immune responses, microscopic mites called Demodex folliculorum (which live on everyone’s skin but multiply too much in rosacea), and messed-up blood vessels. Topical antibiotics like metronidazole, ivermectin, and azelaic acid work by reducing this inflammation, not by killing germs.
Metronidazole has been the go-to for nearly 40 years. It’s affordable, well-studied, and gentle. Applied twice daily, it reduces inflammatory lesions by 60-70% after 6-9 weeks. But it’s not magic. It takes time. And it doesn’t touch the redness or flushing-only the bumps.
Ivermectin, approved in 2014, changed the game. In a 2019 study with 900 patients, ivermectin 1% cream cut lesions by 76% in 12 weeks-better than metronidazole’s 55%. Why? It targets Demodex mites and reduces inflammation at the same time. That dual action makes it more effective for many people. It’s now the top choice for many dermatologists, especially for moderate to severe papulopustular rosacea.
Azelaic acid, while not an antibiotic, works similarly. It reduces redness and bumps with 68-73% effectiveness over 15 weeks. It’s a good option if you’re sensitive to other treatments or want something with fewer side effects. It’s also safe to use during pregnancy, which matters for some patients.
Comparing the Top Treatments
| Treatment | Active Ingredient | Reduction in Lesions | Time to Notice Improvement | Common Side Effects | Best For |
|---|---|---|---|---|---|
| Ivermectin 1% cream | Ivermectin | 76% at 12 weeks | 4-6 weeks | Stinging (22%), dryness | Severe bumps, Demodex involvement |
| Metronidazole 0.75% gel | Metronidazole | 60-70% at 6-9 weeks | 6-8 weeks | Stinging (15%), mild dryness | Mild cases, sensitive skin |
| Azelaic acid 15% gel | Azelaic acid | 68-73% at 15 weeks | 8-12 weeks | Burning, itching (10-15%) | Redness + bumps, pregnancy-safe |
Here’s the thing: no single treatment fixes everything. Ivermectin is the most effective for bumps, but it can sting at first. Metronidazole is gentler but slower. Azelaic acid helps with redness too, but it takes longer. Many people need a combination. Dermatologists now often pair one of these with a redness-reducing cream like brimonidine or oxymetazoline. That’s because topical antibiotics don’t touch the flushing. They only calm the bumps.
Real Results-and Real Struggles
People who’ve tried these treatments say the same thing: patience is everything. On Drugs.com, ivermectin has a 7.2 out of 10 rating. About 62% of users say it helped. But 16% say it made things worse. Why? The first two weeks. Many report increased redness, peeling, or burning. That’s not an allergic reaction-it’s your skin adjusting. One Reddit user wrote: “First two weeks of metronidazole felt like my face was on fire. I almost quit. I’m glad I didn’t.”
Another common complaint? Cost. Without insurance, these creams can run $350 a year. That’s a lot for something you have to use every day for months. And even when you stick with it, results aren’t instant. Most people don’t see improvement until 4-8 weeks in. The National Rosacea Society found that 45% of patients quit within six months because they didn’t see quick results.
Adherence is the biggest hurdle. Only 40-50% of people use their medication consistently beyond three months. That’s why dermatologists stress: start slow. Do a patch test on your jawline for three days before applying it all over. Use a pea-sized amount for your whole face. Too much doesn’t help-it irritates. Apply it to dry skin, 15 minutes after washing. And don’t mix it with harsh toners, retinoids, or scrubs. Your skin barrier is already fragile.
What You Should Do Alongside Treatment
Topical antibiotics alone won’t win the battle. Rosacea is triggered by things you can control. UV exposure is the biggest one. Sunscreen isn’t optional-it’s mandatory. Look for mineral sunscreens with zinc oxide (10-20%). Avoid chemical sunscreens-they can sting. Also avoid alcohol-based toners, fragranced lotions, and foaming cleansers. Stick to gentle, pH-balanced (5.5-7.0) cleansers. Wash with lukewarm water, not hot.
Track your triggers. Keep a simple diary: what you ate, drank, where you were, how hot it was, how stressed you felt. Common triggers include:
- Hot drinks (over 60°C / 140°F)
- Red wine (12-15% alcohol)
- Spicy food (capsaicin above 0.01%)
- Stress and anxiety
- Extreme heat or cold
- UV exposure (UV index above 3)
Many people find that cutting out just one or two triggers makes a huge difference. One patient stopped drinking red wine and noticed flushing dropped by 70%. Another switched from a foaming cleanser to a cream-based one and saw less stinging from her ivermectin.

When Treatment Fails
If after 8 weeks you’ve seen less than 25% improvement, it’s time to talk to your dermatologist. You might need a different medication, a combination approach, or even oral antibiotics like doxycycline for short-term flare-ups. Some people benefit from light therapies like intense pulsed light (IPL), which targets blood vessels and reduces redness. Others need long-term maintenance with lower-dose topical treatments.
And don’t ignore the eyes. Up to 75% of rosacea patients have ocular symptoms-dryness, grittiness, light sensitivity. If your eyes feel irritated, tell your doctor. Left untreated, it can lead to serious eye damage.
What’s Next for Rosacea Treatment
The rosacea market is growing fast-projected to hit $2.74 billion by 2030. New combinations are coming. Galderma is testing a cream that mixes ivermectin with hydrocortisone. Early results show 85% lesion reduction-better than ivermectin alone. That’s promising. But the core truth hasn’t changed: topical antibiotics are still the foundation. They’re safe, effective, and backed by decades of research.
The future isn’t about finding one miracle cure. It’s about personalized care. What works for one person might not work for another. Your skin, your triggers, your lifestyle-all of that matters. The goal isn’t perfection. It’s control. Less flushing. Fewer bumps. More confidence.
Can topical antibiotics cure rosacea?
No, topical antibiotics cannot cure rosacea. Rosacea is a chronic condition with no known cure. These treatments help control symptoms-especially inflammatory bumps and pustules-but they don’t eliminate the underlying causes like vascular dysfunction or immune overactivity. Long-term management is needed, often combining medications with trigger avoidance and gentle skincare.
How long does it take for topical antibiotics to work?
Most people start seeing improvement in 4-8 weeks, but full results usually take 12-16 weeks. Ivermectin tends to work faster than metronidazole, with noticeable changes by week 4-6. Don’t stop treatment just because you don’t see results right away. Consistency matters more than speed.
Do topical antibiotics make rosacea worse at first?
Yes, some people experience a temporary flare-up in the first 1-2 weeks. This can include increased redness, stinging, or dryness. It’s not an allergic reaction-it’s your skin adjusting. Most people tolerate it if they continue. If irritation is severe, talk to your dermatologist about switching to a gentler formulation or using a barrier-repair moisturizer alongside the treatment.
Can I use these treatments if I’m pregnant?
Azelaic acid is considered safe during pregnancy and is often recommended. Metronidazole and ivermectin have limited safety data in pregnancy, so they’re usually avoided unless benefits clearly outweigh risks. Always consult your dermatologist and OB-GYN before starting any new treatment while pregnant or breastfeeding.
What’s the difference between flushing and persistent redness?
Flushing is temporary redness triggered by heat, stress, or alcohol-it comes and goes. Persistent redness (erythema) is constant, even when you’re not triggered. It’s the result of repeated flushing over time, leading to permanently dilated blood vessels. Topical antibiotics help with bumps but not with persistent redness. For that, you need treatments like brimonidine or oxymetazoline.
Is it safe to use topical antibiotics long-term?
Yes. Unlike oral antibiotics, topical versions like metronidazole and ivermectin are designed for long-term use. They don’t cause antibiotic resistance when used correctly on the skin. Side effects are usually mild-dryness or stinging-and occur in less than 25% of users. Long-term use is common and recommended by dermatologists to keep symptoms under control.
Final Thoughts
Rosacea is frustrating, but it’s manageable. You don’t need to live with constant redness and bumps. The right topical antibiotic, paired with trigger awareness and gentle skincare, can transform your skin-and your life. It’s not about perfection. It’s about progress. Start with one change: track your triggers. Then talk to a dermatologist about what treatment fits your skin. You’ve got this.

Jennifer Griffith
November 23, 2025 AT 00:22so i tried ivermectin and my face looked like a tomato for 2 weeks 😭 then it got better?? idk man
Kimberley Chronicle
November 23, 2025 AT 12:17From a clinical perspective, the dual-action mechanism of ivermectin-targeting both Demodex folliculorum and the downstream inflammatory cascade-is a paradigm shift in topical rosacea management. The 76% lesion reduction in the 2019 RCT is statistically significant (p<0.001) and clinically meaningful, especially when compared to metronidazole’s modest 55%. However, the stinging phenotype in 22% of patients suggests a TLR-2-mediated reaction, which may require pre-treatment barrier repair with ceramide-containing emollients.
Pallab Dasgupta
November 24, 2025 AT 20:24bro i was crying in the shower from this stuff burning my face but i stuck with it for 3 months and now i can go outside without feeling like a glowing ghost. this shit works if you dont quit. dont listen to the haters. your skin will thank you later. 💪
prasad gaude
November 24, 2025 AT 22:56It's fascinating how the body's immune system, in its overzealous attempt to protect us, turns against itself. Rosacea, in many ways, is not merely a skin condition-it's a mirror of our internal chaos. The mites? They're just passengers. The real enemy is the storm within: stress, diet, the relentless pace of modern life. We treat the redness, but never the root. Perhaps healing begins not with a cream, but with stillness.
I've seen men in Mumbai, with faces like burnt parchment, walk into clinics begging for relief. They don't know the triggers. They don't know that chai at 70°C is a dagger. They think it's 'bad skin.' But it's deeper. It's a cry for balance.
And yet-we are so quick to blame the skin, never the soul.
Ellen Sales
November 26, 2025 AT 01:51okay so i used azelaic acid and my face looked like i’d been slapped with a brick for 10 days and i thought i was dying but then one day i woke up and it was just… gone? like magic? i cried. i still use it. i’m not even sorry.
Josh Zubkoff
November 26, 2025 AT 07:19Look, I’ve read the entire study, and I’m sorry, but this whole topical antibiotic thing is just a big pharma cash grab. You know what fixes rosacea? Quitting alcohol, stopping your overpriced skincare routine, and not being a hypochondriac who stares at their face in the mirror every 5 minutes. You’re not broken. You’re just a millennial who thinks a $120 cream will fix your anxiety. The real problem? You’re not sleeping. You’re on TikTok. You’re stressed. You’re not washing your pillowcase. You think a cream is going to fix that? Newsflash: your skin isn’t a widget. It’s a reflection of your life choices. And if you’re still using foaming cleansers after reading this? You’re beyond help.
fiona collins
November 27, 2025 AT 03:58Thank you for sharing this. I appreciate the clarity.
giselle kate
November 27, 2025 AT 08:34Why are we even using Western medicine for this? In India, they’ve been using neem and turmeric for centuries. Why are we paying $350 for a tube of cream when a $5 jar of turmeric powder works better? This is cultural imperialism disguised as science. Wake up.
Emily Craig
November 28, 2025 AT 13:09so i used ivermectin and my face looked like i’d been dipped in hot sauce for two weeks but then i got a text from my ex saying they miss me and suddenly my redness was gone? i think love cures rosacea? 🤷♀️
Leisha Haynes
November 28, 2025 AT 14:31you’re not alone. i thought i was the only one crying over a cream. i started with metronidazole, switched to ivermectin, now i’m on azelaic acid and i’ve got a whole skincare altar in my bathroom. but i can finally wear a turtleneck without feeling like a tomato. worth it.
Amy Hutchinson
November 29, 2025 AT 10:22hey i saw your post and i have rosacea too!! can i ask what brand sunscreen you use?? i tried the zinc one and it left a white cast and i felt like a ghost 😭
Erika Hunt
December 1, 2025 AT 09:55It’s interesting how we’ve pathologized something so fundamentally human-blushing. Rosacea isn’t a disease of the skin, it’s a disease of exposure. We live in a world that demands we look perfect, feel calm, and never show vulnerability. But our skin remembers every stress, every hot drink, every judgmental glance. The redness isn’t a flaw-it’s a message. Maybe we need to stop trying to erase it, and start listening to it.
I’ve noticed that when I meditate for even 10 minutes a day, the flushing slows. Not because of any chemical, but because I’m no longer screaming inside. The cream helps, yes. But peace? That’s the real treatment.
And yet, we still treat skin like a surface to be polished, not a language to be understood.
Lisa Odence
December 3, 2025 AT 04:01As a board-certified dermatologist with 18 years of clinical experience, I must emphasize that the data supporting ivermectin’s efficacy is robust, with a number needed to treat (NNT) of 2.3 for >75% reduction in papulopustules at 12 weeks. However, the cost-benefit analysis must be considered, particularly in uninsured populations. I recommend combining ivermectin with a low-dose, non-comedogenic moisturizer containing niacinamide (5%) to mitigate initial irritation. Also, please avoid using retinoids concurrently, as this may compromise the stratum corneum barrier. 🌿
Rachel Villegas
December 3, 2025 AT 16:02I’ve been using metronidazole for 6 months. My skin isn’t perfect, but I don’t hide in my house anymore. That’s enough.
Srikanth BH
December 5, 2025 AT 15:15Hey, if you’re struggling-keep going. It’s not easy. But every day you stick with it, your skin gets a little lighter. I used to avoid mirrors. Now I look at myself and say, ‘you’re still here.’ And that’s victory.
Shirou Spade
December 6, 2025 AT 06:22There’s a quiet violence in how we treat our bodies-chasing perfection with chemicals, ignoring the signals they send. Rosacea doesn’t care about your Instagram aesthetic. It responds to silence, to rest, to the absence of judgment. Maybe the real treatment isn’t in the tube-but in the pause between breaths.
Karen Willie
December 8, 2025 AT 04:44If you're new to this, start with sunscreen and a gentle cleanser. That’s it. No need to buy 7 creams. Your skin just needs space to breathe.