Medication Timing: When to Take Drugs for Best Results
When you take a medication isn't just a habit—it's a medication timing, the precise schedule at which drugs are absorbed, metabolized, and activated in the body. Also known as dosing intervals, it can make the difference between a drug working well or causing avoidable side effects. Many people pop pills with breakfast, before bed, or whenever they remember—but that’s not how pharmacology works. The body has rhythms. Your stomach acid changes throughout the day. Liver enzymes peak at certain hours. Blood pressure naturally dips at night. And if you’re taking something like a blood thinner, a statin, or an antibiotic, missing the right window can reduce its power—or even put you at risk.
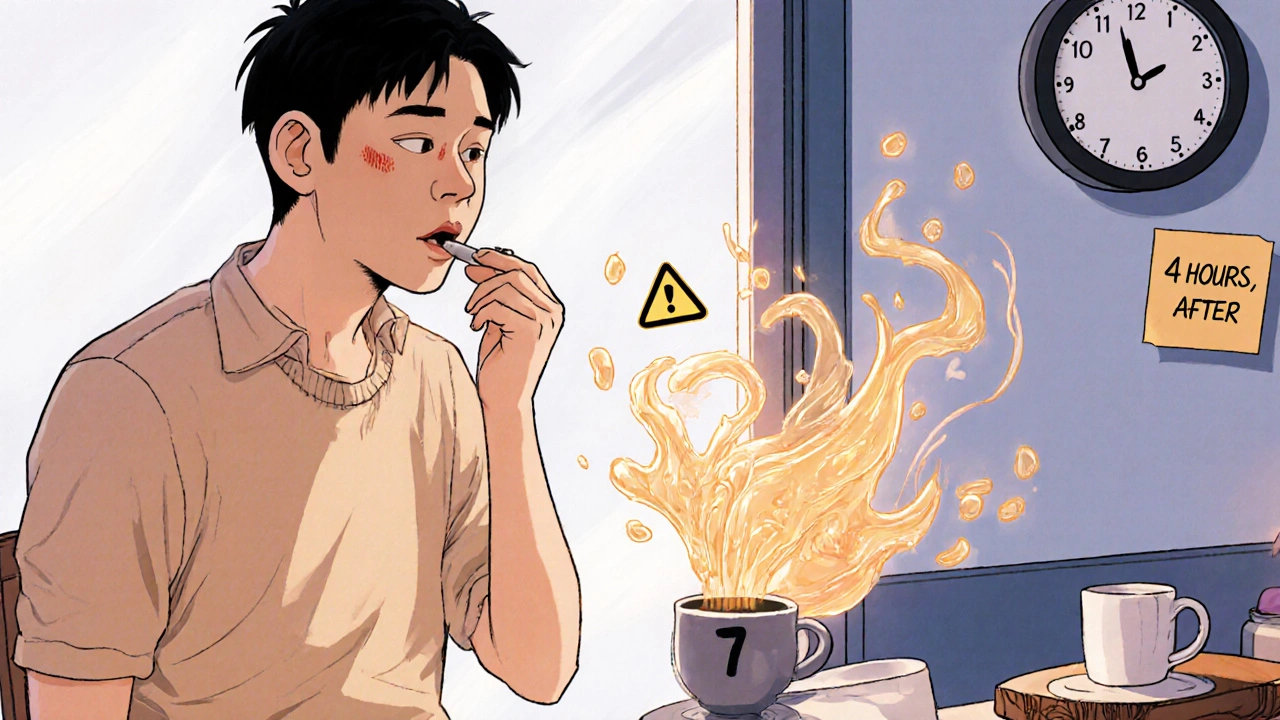
For example, drug absorption, how quickly and completely a medication enters your bloodstream depends heavily on whether you take it with food or on an empty stomach. Some antibiotics, like doxycycline, bind to calcium in dairy and become useless if taken with milk. Others, like statins, work better at night because your liver produces most cholesterol while you sleep. Then there’s medication side effects, unwanted reactions that often depend on when the drug peaks in your system. A stimulant taken too late can wreck your sleep. A diuretic taken after 4 p.m. might mean midnight bathroom trips. Even something as simple as aspirin can irritate your stomach more if taken without food.
Timing also affects how well your body tolerates long-term use. Taking thyroid meds like levothyroxine on an empty stomach, 30 to 60 minutes before breakfast, isn’t a suggestion—it’s a requirement for stable hormone levels. Skipping that window can throw off your whole metabolic balance. And when it comes to antibiotics, hitting the exact dosing interval—every 8 or 12 hours—keeps enough of the drug in your system to kill bacteria without letting them adapt. Miss a dose? Stretch it to 14 hours? You’re not just being lazy—you’re risking treatment failure and antibiotic resistance.
It’s not just about the drug, either. It’s about you. Your job, your sleep schedule, your meals, your other meds. A pill that works perfectly for one person might cause dizziness in another simply because they take it before driving. That’s why the best medication timing isn’t generic—it’s personalized. And the posts below show exactly how this plays out in real life: from how Bupropion affects energy levels when taken in the morning, to why pregnant women need trimester-specific timing for migraine relief, to how statins, antihypertensives, and even acne creams behave differently depending on when they’re taken. You’ll find practical, no-fluff advice on avoiding dangerous interactions, reducing side effects, and making your meds actually work. No guesswork. Just clear, science-backed timing rules you can use today.