Muscle relaxant — when to use, how they work, and safety tips
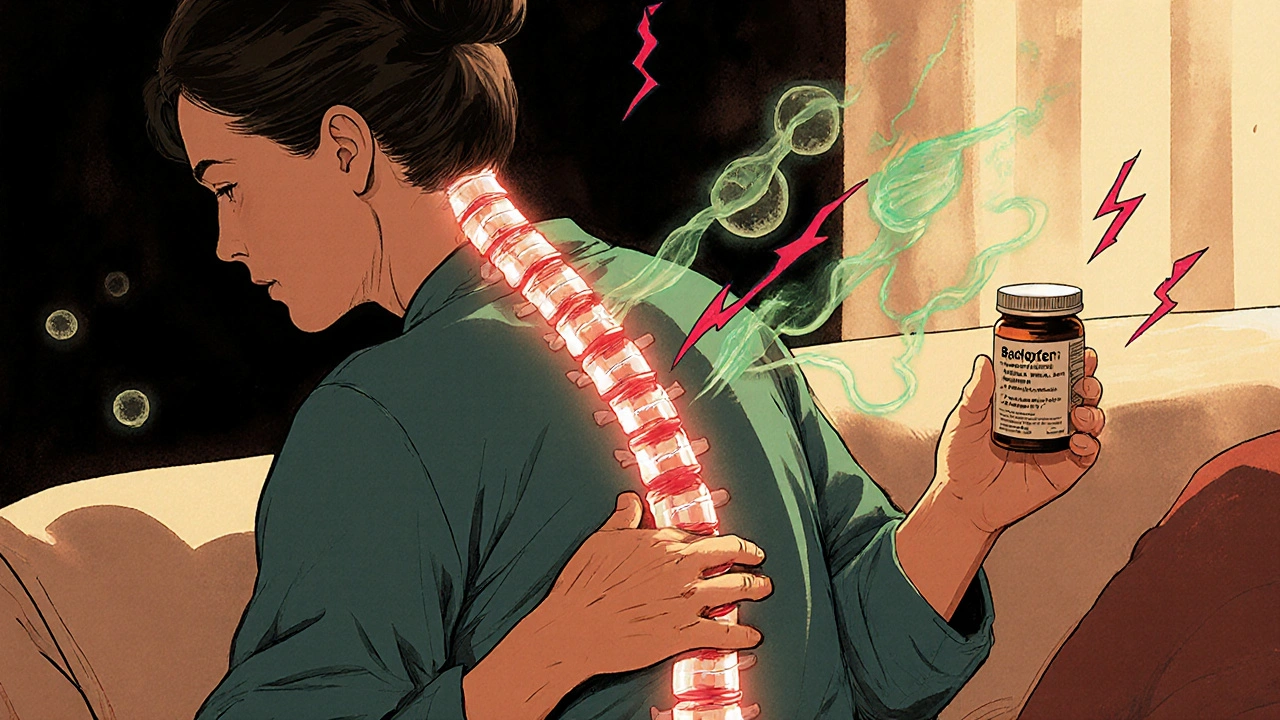
Muscle relaxants are medicines that ease painful muscle tightness and spasms. People get them for back pain, neck strains, sciatica, or after surgery. Some work by acting on the spinal cord and brain (central muscle relaxants) and others by acting on the muscle itself. Knowing how each type works helps you pick the right option and avoid surprises.
Common names you’ll hear: cyclobenzaprine, tizanidine, baclofen, methocarbamol and carisoprodol. These differ in speed, side effects and how long they last. For short-term muscle spasm after an injury, cyclobenzaprine or methocarbamol often help quickly. If spasticity from a neurological condition is the problem, doctors may reach for baclofen. Tizanidine can calm severe spasms but may lower blood pressure.
What to watch for
Most muscle relaxants cause drowsiness, dizziness, or lightheadedness. Mixing them with opioids, benzodiazepines, or alcohol can dangerously increase sedation and slow breathing. They can also cause dry mouth, blurred vision, or trouble concentrating. Older adults tend to feel side effects more, so lower doses or different choices are usually safer.
Don't use muscle relaxants while driving or operating machines until you know how you react. If you start new symptoms like fast heartbeat, severe weakness, breathing trouble, or fainting, seek medical help right away. Also mention any liver or kidney problems to your prescriber — some drugs need dose changes or extra monitoring.
Practical tips for treatment and buying
Start with non-drug options: rest, targeted stretches, heat or cold packs, and a short course of physical therapy. Muscle relaxants are best for short bursts (days to a few weeks) unless a doctor prescribes long-term treatment for spasticity. If you need ongoing help, ask about alternatives like baclofen pumps, botulinum toxin injections, or physical rehab programs.
Thinking of buying meds online? Only use pharmacies that ask for a valid prescription and show clear contact details, licensing, and pharmacist access. Avoid sites that sell controlled or prescription drugs without a prescription. Keep receipts, check packaging for tampering, and compare prices across reputable pharmacies. If a deal looks too good, it probably is.
Pregnancy, breastfeeding, and children require special caution — many muscle relaxants are not recommended and some cross into breast milk. If you have upcoming surgery, tell the anesthetist about any muscle relaxant use; some drugs change anesthesia needs and recovery. For chronic problems, don’t rely only on pills. Combine guided exercise, posture work, and ergonomic fixes at work. If pain keeps returning, a focused evaluation—such as imaging or a neurologic review—can find underlying causes like nerve impingement that need different treatment than muscle relaxants.
When you talk to your doctor or pharmacist, be specific: list other meds, alcohol use, sleep issues, and any history of addiction. Ask how long to take the drug, what to expect in the first 48 hours, and when to stop it. Keep notes on what helps and share them with your clinician. A clear plan cuts down risks and helps you get back to normal faster.