Targeted Therapy for Advanced Renal Cell Carcinoma: Current Role and 2025 Outlook
 Oct, 12 2025
Oct, 12 2025
Treatment Selection Calculator for Advanced RCC
Select patient factors to see treatment options
Key Takeaways
- Targeted therapy now forms the backbone of first‑line treatment for advanced renal cell carcinoma (RCC).
- Tyrosine‑kinase inhibitors (TKIs) and immune checkpoint inhibitors (ICIs) are most often combined to improve response rates.
- Biomarker testing - especially for VHL, MET, and PD‑L1 - helps clinicians tailor the regimen.
- Managing side effects early keeps patients on therapy longer and boosts overall survival.
- Emerging agents targeting HIF‑2α and novel combinations are reshaping the 2025 treatment landscape.
When a kidney cancer reaches an advanced stage, the treatment landscape has changed dramatically over the past decade. What makes renal cell carcinoma so challenging is its tendency to grow blood vessels rapidly and to resist conventional chemotherapy. Nowadays, doctors rely on targeted drugs that zero in on the molecular pathways driving those tumors.
Advanced renal cell carcinoma is a late‑stage kidney cancer that has spread beyond the kidney. It represents roughly 75% of kidney‑cancer diagnoses worldwide and accounts for a high proportion of cancer‑related deaths.
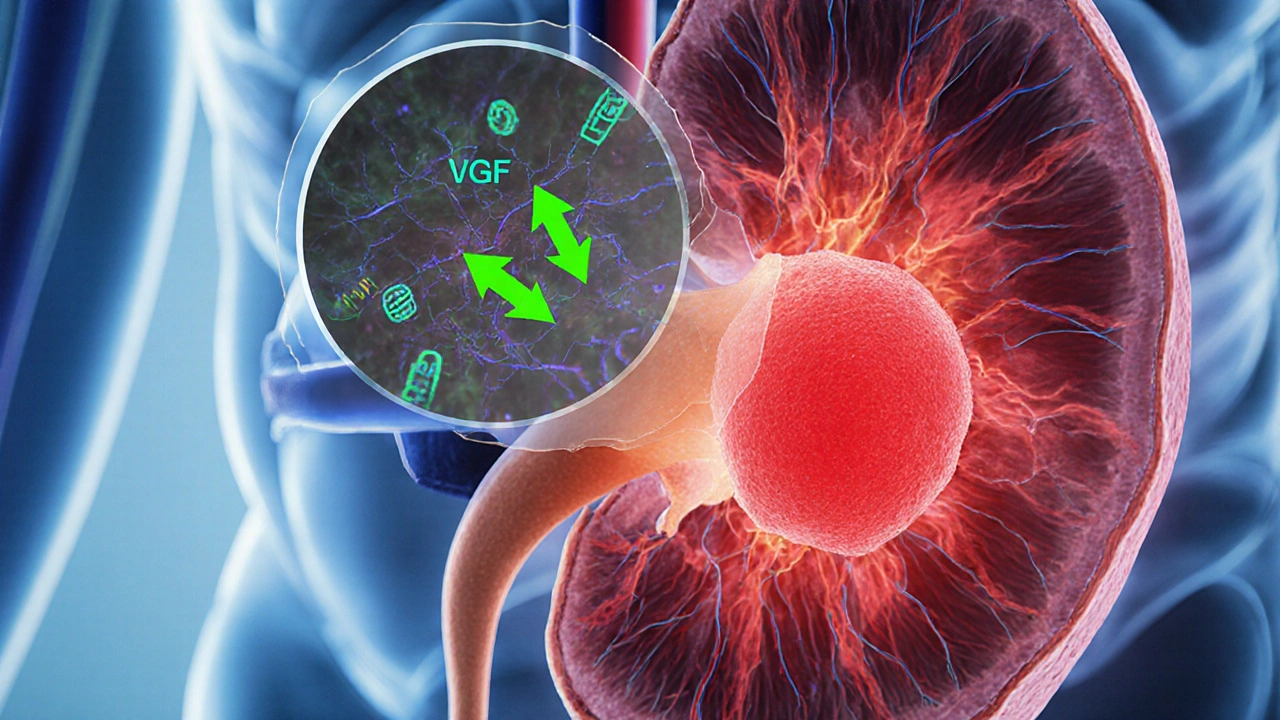
Understanding the disease biology
RCC is not a single disease; it comprises several histologic subtypes, with clear‑cell RCC (ccRCC) being the most common. The VHL gene, which normally degrades hypoxia‑inducible factor (HIF), is frequently mutated. Loss of VHL leads to unchecked HIF activity, which in turn ramps up vascular endothelial growth factor (VEGF) production. This explains why the tumours are so vascular.
Beyond VHL, other pathways such as MET, AXL, and the mammalian target of rapamycin (mTOR) play supporting roles. These molecular insights are the reason targeted agents work so well - they interrupt the exact signals the tumour depends on.
What is targeted therapy?
Targeted therapy refers to drugs designed to block specific molecules involved in cancer growth. In RCC, the three main families are:
- Tyrosine‑kinase inhibitors (TKIs) that block VEGF receptors, PDGFR, and sometimes MET.
- Immune checkpoint inhibitors (ICIs) that unleash T‑cells by blocking PD‑1, PD‑L1, or CTLA‑4.
- mTOR inhibitors that disrupt a downstream growth‑promoting pathway.
Each class attacks the tumour from a different angle, and the newest regimens combine them for synergistic effect.
Key drug classes used today
Tyrosine‑kinase inhibitors are oral pills that inhibit VEGF‑driven angiogenesis. Common agents include sunitinib, pazopanib, axitinib, and the newer lenvatinib.ICIs such as pembrolizumab, nivolumab, and the combination ipilimumab+nivolumab have transformed survival, especially when paired with a TKI.
mTOR inhibitors - everolimus and temsirolimus - are less frequently first‑line but remain valuable after progression on TKI/ICI combos.| Class | Mechanism | First FDA approval (year) | Typical response rate* | Common side effects |
|---|---|---|---|---|
| TKI | Blocks VEGFR, PDGFR, sometimes MET | 2006 (sunitinib) | 30‑40% | Hypertension, diarrhea, hand‑foot skin reaction |
| ICI | Inhibits PD‑1/PD‑L1 or CTLA‑4 checkpoints | 2015 (nivolumab) | 20‑35% (higher when combined with TKI) | Immune‑related colitis, pneumonitis, thyroiditis |
| mTOR inhibitor | Blocks mTORC1 signaling downstream of PI3K/AKT | 2008 (temsirolimus) | 15‑20% | Hyperglycemia, stomatitis, fatigue |
How clinicians pick the right regimen
The decision isn’t random. Doctors start with a set of biomarkers and patient‑specific factors:
- PD‑L1 expression - higher levels often predict better ICI response.
- MET alterations - guide use of cabozantinib or lenvatinib.
- Performance status (ECOG score) - determines how aggressive therapy can be.
- Comorbidities such as cardiovascular disease, which influence TKI choice.
In 2024‑2025, the most common first‑line combos are:
- Pembrolizumab+axitinib
- Nivolumab+cabozantinib
- Lenvatinib+pembrolizumab (approved for patients with high‑risk disease).
These pair an ICI with a TKI, delivering median overall survival beyond 4 years in pivotal trials.
Managing side effects - the pragmatic part
Targeted drugs are powerful, but they come with a cost. Early detection and dose adjustment keep patients on therapy:
- Hypertension - monitor blood pressure weekly for the first two months; start ACE inhibitors if needed.
- Diarrhea - loperamide 2mg after the first loose stool, then every 2hours as required.
- Immune‑related colitis - hold the ICI at grade≥2, start prednisone 1mg/kg, taper over 4‑6weeks.
- Hand‑foot skin reaction - moisturize daily, avoid heat; dose‑reduce TKI if grade3.
Multidisciplinary clinics involving oncologists, nurses, and pharmacists have shown a 15% reduction in treatment discontinuation rates.
Emerging options and what 2025 may bring
Research isn’t standing still. Two developments are already reshaping practice:
- HIF‑2α inhibitors - belzutifan received accelerated approval in 2023 for VHL‑associated RCC and is now being tested in broader advanced RCC populations. Early data show a 45% objective response rate with a manageable safety profile.
- Novel triplet combos - trials combining an ICI, a TKI, and a HIF‑2α inhibitor aim to achieve deeper, more durable remissions.
Liquid biopsy techniques are also gaining traction. Detecting circulating tumor DNA (ctDNA) allows clinicians to spot resistance mutations (e.g., VEGFR2 or MET) before radiologic progression, enabling a pre‑emptive switch to a more effective agent.
Practical checklist for clinicians and patients
- Confirm histology and stage with imaging and pathology.
- Order baseline labs: CBC, CMP, thyroid panel, and VEGF‑related biomarkers.
- Discuss therapeutic goals (life‑extension vs. symptom control).
- Choose a regimen based on PD‑L1, MET status, and comorbidities.
- Set up a side‑effect monitoring schedule: BP weekly, skin exam every visit, labs every 4‑6weeks.
- Plan for imaging re‑assessment at 12weeks, then every 8‑12weeks.
- Keep a log of symptoms and medication adherence - it helps the care team intervene early.
Frequently Asked Questions
Can targeted therapy cure advanced RCC?
Complete cure is still rare, but modern combinations can turn a rapidly progressive disease into a chronic condition with several years of survival. Long‑term remission is seen in a minority of patients, especially those with favorable biomarkers.
Do I need genetic testing before starting treatment?
Testing for VHL, MET alterations, and PD‑L1 expression is now recommended by most guidelines. The results help tailor the TKI or decide whether an ICI‑dominant regimen is preferable.
What are the most common side effects of the pembrolizumab+axitinib combo?
Patients often experience hypertension, diarrhea, and fatigue from axitinib, plus rash, thyroid dysfunction, or mild colitis from pembrolizumab. Most issues are manageable with dose adjustments and symptomatic treatment.
How often should imaging be done to assess response?
A baseline scan is followed by a reassessment at roughly 12weeks. If disease is stable, subsequent scans every 8‑12weeks are typical, unless symptoms dictate earlier imaging.
Are there special considerations for older patients?
Yes. Age‑related comorbidities (heart disease, renal impairment) may limit the use of certain TKIs. Starting at a lower dose and titrating up, while closely monitoring labs, can maintain efficacy while reducing toxicity.

Adam Martin
October 12, 2025 AT 19:25Sure, because we totally need another calculator to decide which drug to throw at kidneys.
Ryan Torres
October 14, 2025 AT 13:05Big Pharma's secret agenda is obvious – they want us all glued to overpriced IV drips while they line their pockets, so they slap on a new combo therapy every quarter 😒💊. The whole "targeted" hype is just a smoke screen for endless clinical trial enrollment.
shashi Shekhar
October 16, 2025 AT 06:45Yeah, because waiting for the next breakthrough while juggling side effects is exactly what every patient signed up for. The whole spiel about "personalized medicine" feels more like a marketing gimmick than actual progress.
Marcia Bailey
October 18, 2025 AT 00:25Hey team, just wanted to share that incorporating regular blood pressure checks and skin assessments can really help patients tolerate the VEGF inhibitors longer. A proactive approach often reduces dose interruptions and keeps the treatment on track. Keep up the great work! :)
Hannah Tran
October 19, 2025 AT 18:05When we talk about the next frontier of RCC management, the terminology alone-immune checkpoint inhibition combined with VEGF pathway blockade-already sounds like sci‑fi jargon.
Yet the data from the 2023 CLEAR and CheckMate-9ER trials prove that this is not just hype but a tangible shift in overall survival curves.
Patients with high PD‑L1 expression derive a statistically significant hazard ratio reduction when given pembrolizumab plus lenvatinib, pushing median OS beyond four years.
Conversely, the low PD‑L1 cohort still benefits, albeit modestly, from cabozantinib monotherapy, highlighting the need for biomarker‑driven personalization.
From a pharmacodynamic standpoint, the dual inhibition of VEGFR and MET pathways synergizes with T‑cell activation, attenuating tumor angiogenesis while unshackling the immune microenvironment.
One must also reckon with the toxicity profile; grade 3–4 hypertension and hand‑foot syndrome are not trivial and often mandate dose reductions.
Nevertheless, proactive management-incorporating antihypertensives early and patient‑reported outcome tools-can mitigate discontinuations.
Real‑world registries are already reporting adherence rates above 80%, suggesting that clinicians are getting better at balancing efficacy and safety.
Looking ahead to 2025, the pipeline boasts novel bispecific antibodies that simultaneously target PD‑L1 and VEGFR‑2, potentially condensing combination regimens into a single agent.
Early phase I data indicate manageable safety signals, but long‑term follow‑up will be crucial to confirm durability.
In addition, the emergence of circulating tumor DNA as a liquid biopsy could refine our selection criteria beyond static tissue PD‑L1 measurements.
Integrating ctDNA dynamics might allow us to switch therapies preemptively before radiographic progression.
Economic considerations cannot be ignored; the cost‑effectiveness analyses favor regimens with the highest quality‑adjusted life years per dollar, especially when generic TKIs become available.
Health systems should therefore negotiate risk‑sharing agreements to ensure broader patient access.
In summary, the therapeutic landscape for advanced RCC is evolving from sequential monotherapies to rationally designed, biomarker‑guided combos, and staying updated on trial data will be essential for optimal patient outcomes.
Crystle Imrie
October 21, 2025 AT 11:45Another day, another "breakthrough" that costs a fortune. The drama never ends.
Shelby Rock
October 23, 2025 AT 05:25i wonder if the universe kinda whispers that all these meds are just a way to keep us busy while the real cure is some ancient herb we forgot.
Alex Iosa
October 24, 2025 AT 23:05From an ethical standpoint, the rapid rollout of combination regimens without long‑term safety data raises concerns about informed consent, especially when patients are presented with optimistic survival figures that may not reflect individual variability.
melissa hird
October 26, 2025 AT 15:45Ah, the grand tradition of Western oncology-sprinkling the latest molecular buzzwords over a patient’s chart while the real humanity gets lost in a sea of acronyms. One can only admire the commitment to style over substance.
Abraham Gayah
October 28, 2025 AT 09:25Honestly, the whole circus of layering checkpoint inhibitors on top of TKIs feels like trying to dress a horse in a tuxedo-impressive at first glance but completely unnecessary for the real work.
rajendra kanoujiya
October 30, 2025 AT 03:05While everyone's busy chanting about combinations, it's worth noting that some patients simply do fine on monotherapy, and the push for more drugs can sometimes be more about market share than medicine.