Aspirin for Primary Prevention: Who Should Skip Daily Doses
 Jan, 8 2026
Jan, 8 2026
For years, taking a daily low-dose aspirin was seen as a simple, cheap way to prevent a first heart attack or stroke. Many people over 50 popped one every morning, thinking they were protecting their heart. But the science has changed. Aspirin is no longer recommended for most healthy adults as a routine preventive measure. In fact, for many, it’s doing more harm than good.
Why the Change? The Risks Outweigh the Benefits
The idea behind daily aspirin was simple: aspirin thins the blood, so it might stop clots from forming in arteries and causing heart attacks or strokes. Early studies in the 1980s and 90s showed a small benefit. But those studies didn’t fully account for the bleeding risks - and we now know those risks are real, serious, and grow with age.
Today, the data is clear. For people without existing heart disease, the chance of avoiding a heart attack with aspirin is tiny - about 1 in 1,000 people per year. Meanwhile, the risk of a major bleed - like a stomach ulcer that won’t stop bleeding or a brain hemorrhage - is higher than that. In adults over 60, for every 1,000 people taking aspirin daily for a year, you get about 0.9 fewer heart attacks but 1.6 more major bleeds. That’s not a trade-off worth making.
The U.S. Preventive Services Task Force (USPSTF) updated its guidelines in 2022 and now says: do not start aspirin for primary prevention if you’re 60 or older. The American Heart Association and American College of Cardiology agree. Even in younger adults, it’s not a blanket recommendation. It’s a personal decision - and only if you’re at high enough risk of heart disease and low enough risk of bleeding.
Who Should Absolutely Skip Daily Aspirin?
Not everyone is at equal risk. Some people should never take daily aspirin - even if they’re young and healthy.
- Anyone over 60 without known heart disease. This is the clearest group. The bleeding risk climbs sharply after 60. Your stomach lining gets thinner. Blood vessels become more fragile. The small benefit of preventing a heart attack doesn’t balance the high chance of a life-threatening bleed.
- People with a history of stomach ulcers or GI bleeding. Aspirin irritates the stomach lining. If you’ve had a bleeding ulcer before, taking aspirin again raises your risk of another bleed by up to 40%. Even if you’ve never had one, if you’ve had persistent heartburn or use NSAIDs like ibuprofen regularly, you’re at higher risk.
- People taking blood thinners like warfarin, apixaban, or rivaroxaban. Combining aspirin with these drugs multiplies your bleeding risk. You’re not adding protection - you’re adding danger.
- People with uncontrolled high blood pressure. High blood pressure weakens blood vessel walls. Add aspirin, and you increase the chance of a brain bleed. Controlling blood pressure comes first - not aspirin.
- People with liver or kidney disease. These organs help process and clear aspirin from your body. If they’re not working well, aspirin builds up, increasing side effects and bleeding risk.
- Anyone allergic to aspirin or with asthma triggered by NSAIDs. This isn’t just a rash. It can cause severe breathing problems or anaphylaxis.
Who Might Still Consider It? (And Only After a Deep Talk With Your Doctor)
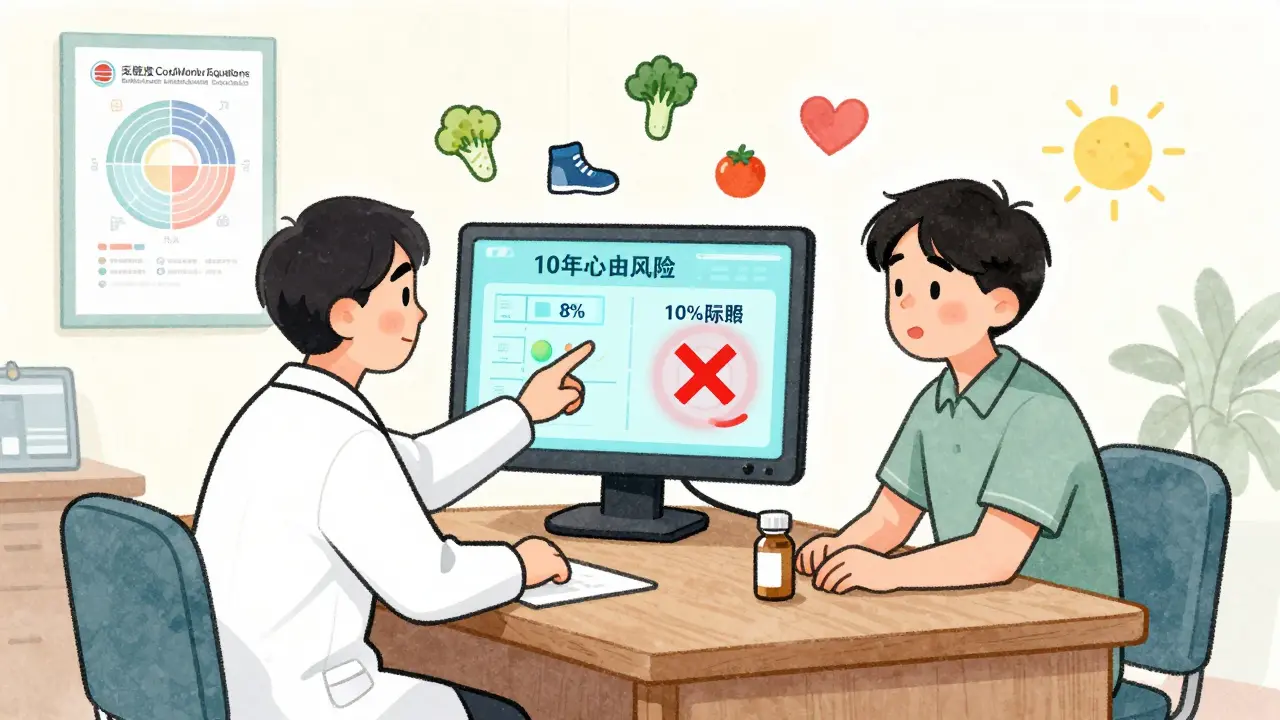
There are exceptions - but they’re narrow. Aspirin might be considered for adults aged 40 to 59 only if all these conditions are true:
- You have a 10% or higher risk of having a heart attack or stroke in the next 10 years.
- You have no increased risk of bleeding.
- You’re willing to take it daily for at least 10 years.
- You’ve discussed it with your doctor and understand the trade-offs.
How do you know your 10-year risk? Your doctor can calculate it using the Pooled Cohort Equations, which look at your age, sex, race, cholesterol, blood pressure, diabetes status, and smoking habits. If your score is below 10%, aspirin won’t help you.
Some people with high calcium scores in their heart arteries (CAC > 100) may benefit even if their overall risk is borderline. But this isn’t automatic. A 2023 study in JAMA Internal Medicine found that among people with CAC scores over 300, those who stopped aspirin after the new guidelines had a 12% higher chance of having their first heart attack. That’s why some cardiologists still recommend it in these specific cases - but only after careful review.
People with type 2 diabetes aged 40-70 and a 10-year ASCVD risk of 15% or higher may also be candidates. But even here, bleeding risk must be low. A 2024 meta-analysis showed aspirin only helped diabetic patients with high Lp(a) levels - a genetic risk factor for heart disease. If your Lp(a) is normal, aspirin likely won’t help.
What About People Who’ve Been Taking It for Years?
Many people - especially those over 60 - have been taking aspirin for 10, 15, or even 20 years. They’re scared to stop. They think, “What if I have a heart attack tomorrow?”
That fear is understandable. But the data says: if you’re over 60 and healthy, stopping aspirin won’t suddenly make you more likely to have a heart attack. In fact, you’re likely reducing your risk of a dangerous bleed.
A 2023 Mayo Clinic survey found 41% of adults 60+ were still taking aspirin for prevention - even after the guidelines changed. Why? Fear. Confusion. And doctors giving mixed messages.
Don’t stop cold turkey. Talk to your doctor. If you’re on a low dose (81 mg), they might suggest tapering off slowly. Stopping abruptly can, in rare cases, trigger a rebound clotting effect. But for most people, stopping is safe and beneficial.
Why Are Doctors Still Confused?
Here’s the messy part: not all doctors are on the same page. Cardiologists are more likely to continue aspirin for high-risk patients than primary care doctors. A 2023 study in JAMA Internal Medicine found that 57% of patients reported getting conflicting advice from different doctors.
Some cardiologists still follow older guidelines or rely on individual cases - like a patient with a CAC score of 500 or a family history of early heart attacks. Others point to the ASPREE trial, which showed no net benefit in seniors, but had high dropout rates and was criticized for its methods.
Meanwhile, primary care doctors are under pressure to make quick decisions. It takes over 7 minutes to properly calculate CVD risk and bleeding risk - and most visits are 10-15 minutes long. So many just keep prescribing aspirin because it’s easier than having a complex conversation.

What Should You Do Instead?
If you’re not taking aspirin for primary prevention, what should you do to protect your heart?
- Know your numbers. Check your blood pressure, cholesterol, and blood sugar. High numbers mean higher risk - and you can fix them.
- Move more. Just 150 minutes of brisk walking a week cuts heart disease risk by 30%.
- Quit smoking. Smoking is the single biggest preventable cause of heart attacks. Quitting cuts your risk in half within a year.
- Eat better. Focus on vegetables, whole grains, nuts, fish, and olive oil. Reduce processed foods, sugar, and salt.
- Maintain a healthy weight. Losing 5-10% of your body weight can dramatically improve blood pressure and cholesterol.
- Ask about Lp(a) testing. If you have a strong family history of early heart disease, ask your doctor if you should get tested. High Lp(a) is genetic and not affected by diet or statins - but it tells you your risk is higher than your cholesterol numbers suggest.
These steps work better than aspirin. They don’t cause bleeding. They don’t cost money. And they help your whole body - not just your heart.
Final Takeaway: Aspirin Isn’t a Magic Bullet
Aspirin was once seen as a wonder drug for the heart. Now we know it’s a tool - and a risky one. For most people, especially those over 60, it’s not worth the danger. The real heart protection comes from lifestyle, not pills.
If you’re unsure whether you should be on aspirin, don’t guess. Don’t rely on old habits. Talk to your doctor. Ask: “What’s my 10-year risk? What’s my bleeding risk? Does the math still work for me?”
There’s no one-size-fits-all answer. But for the vast majority of healthy adults, skipping daily aspirin is the smarter, safer choice.
Should I stop taking aspirin if I’ve been on it for years?
If you’re over 60 and taking aspirin only for primary prevention (no history of heart attack, stroke, stent, or bypass), yes - you should talk to your doctor about stopping. The risks of bleeding now outweigh the small benefit. Don’t stop abruptly; ask your doctor for a safe plan. If you’re under 60 with high heart disease risk and low bleeding risk, you may still benefit. Always check with your provider.
Is baby aspirin safer than regular aspirin?
Yes, low-dose aspirin (75-100 mg, often called "baby aspirin") is the only dose recommended for prevention. Higher doses don’t offer more protection but increase bleeding risk. Even at low doses, the bleeding risk remains significant in older adults. The dose isn’t the issue - it’s whether you need it at all.
Can I take aspirin only a few times a week instead of daily?
No. Aspirin’s anti-clotting effect lasts only a few days, but it also causes ongoing irritation to the stomach lining. Taking it sporadically doesn’t reduce bleeding risk - and likely doesn’t help prevent heart attacks either. If you’re going to take it, it’s daily - or not at all. There’s no proven middle ground for primary prevention.
What if I have a family history of heart disease?
Family history raises your risk - but it doesn’t automatically mean you need aspirin. Your doctor should calculate your 10-year risk using your age, cholesterol, blood pressure, and other factors. If your risk is below 10%, aspirin won’t help. If it’s above 10% and you’re under 60, it might be considered - but only if you have no bleeding risks. Genetic tests like Lp(a) can add clarity, but they don’t replace a full risk assessment.
Are there natural alternatives to aspirin for heart protection?
There’s no natural supplement that replaces aspirin’s blood-thinning effect. But lifestyle changes do - and they’re safer. Eating omega-3-rich fish, getting regular exercise, managing stress, and controlling blood pressure and cholesterol all reduce heart attack risk without the bleeding danger. Turmeric, garlic, and ginger have mild anti-inflammatory effects, but none have been proven to prevent heart attacks like aspirin once did. Don’t trade one unproven supplement for another - focus on what works: movement, food, and medical management.

Maggie Noe
January 10, 2026 AT 13:44Aspirin? Nah. I stopped mine last year after reading this stuff. My grandma lived to 92 without ever popping a pill-just walked every day, ate veggies, and laughed a lot. 🌿❤️
Aron Veldhuizen
January 11, 2026 AT 13:51Let’s be honest: this is just Big Pharma’s latest attempt to sell you a new narrative while quietly letting their billion-dollar anticoagulant market implode. The real story? Doctors are lazy, guidelines are political, and ‘primary prevention’ is a euphemism for ‘we don’t know what else to do.’
And yet, you’ll still find cardiologists prescribing it like it’s coffee. The science? It’s always been messy. But the profit? That’s crystal clear.
Meghan Hammack
January 12, 2026 AT 02:22Hey, if you’ve been taking aspirin for years and are scared to stop-you’re not alone. I was too. But my doc sat with me for 20 minutes, ran the numbers, and said, ‘You’re good to stop.’ I did. No heart attack. No bleed. Just peace of mind. You got this. 💪
Johanna Baxter
January 12, 2026 AT 10:37Someone’s gonna die because they listened to this. Just wait. Someone’s mom will have a stroke next month and it’ll be ‘oh I stopped the aspirin like the internet said.’
And then we’ll all watch another grieving family get roasted by commenters who think they’re doctors now.
Jerian Lewis
January 14, 2026 AT 00:24I’m 58. Took it for 15 years. Stopped last year. No issues. My doctor said it was fine. I didn’t need it. I feel better not taking random pills.
tali murah
January 15, 2026 AT 20:50Oh, so now we’re trusting ‘guidelines’ written by bureaucrats who’ve never met a patient? Brilliant. Meanwhile, real people with CAC scores over 500 are being told to ‘skip aspirin’ while their arteries turn to concrete. The science isn’t settled-it’s being weaponized for liability avoidance.
And yes, I know you’ll quote ASPREE. But that trial had a 40% dropout rate. That’s not data. That’s noise.
Jenci Spradlin
January 17, 2026 AT 19:14my doc said i dont need it anymore but i was scared so i asked for a cac scan. turned out my score was 87. he said ‘you’re fine, stop it.’ i did. no more stomach issues. life’s good. ps: i walk 6k steps daily and eat avo on toast. not magic, just smart.
Micheal Murdoch
January 18, 2026 AT 07:56Let’s zoom out for a second. This isn’t really about aspirin. It’s about how we think about health. We’ve been sold this idea that a pill can fix everything-that we can outsource our well-being to a pharmacy. But the truth? The real medicine is in your kitchen, your shoes, your breath, your sleep. Aspirin was a Band-Aid on a broken system.
And now we’re being asked to see that. It’s uncomfortable. It’s hard. It means admitting we’ve been misled. But that’s growth. That’s maturity. That’s how we become the kind of people who don’t need pills to be healthy.
So if you’re reading this and you’re scared to stop? That’s okay. But ask yourself: what are you really afraid of? The heart attack? Or the idea that you’re responsible for your own health?
There’s no shame in needing help. But there’s power in knowing you’re not powerless.
Drew Pearlman
January 18, 2026 AT 10:42Look, I get it. I used to take it every day. I thought I was being proactive. Turns out I was just following a habit that started in 2008 because my uncle said it was ‘good for circulation.’ Turns out, he was wrong. I didn’t even know what my blood pressure was until I was 55. That’s the real problem-we treat health like a checklist, not a relationship. You don’t fix your heart by swallowing a pill. You fix it by showing up-for yourself, every day. Walking. Eating real food. Sleeping. Laughing. Not taking aspirin because someone told you to. Taking care because you love yourself enough to try. That’s the real win. And it doesn’t come in a bottle.