Chronic Fatigue Syndrome (ME/CFS): What to Watch For and What to Do
Feeling exhausted even after a full night’s sleep? If your energy crashes after light activity and rest doesn’t help, that pattern—called post-exertional malaise (PEM)—is the red flag people with chronic fatigue syndrome (ME/CFS) mention first. An estimated 1–2 million Americans live with ME/CFS. You don’t have to accept constant exhaustion; there are clear steps that help many people feel better day to day.
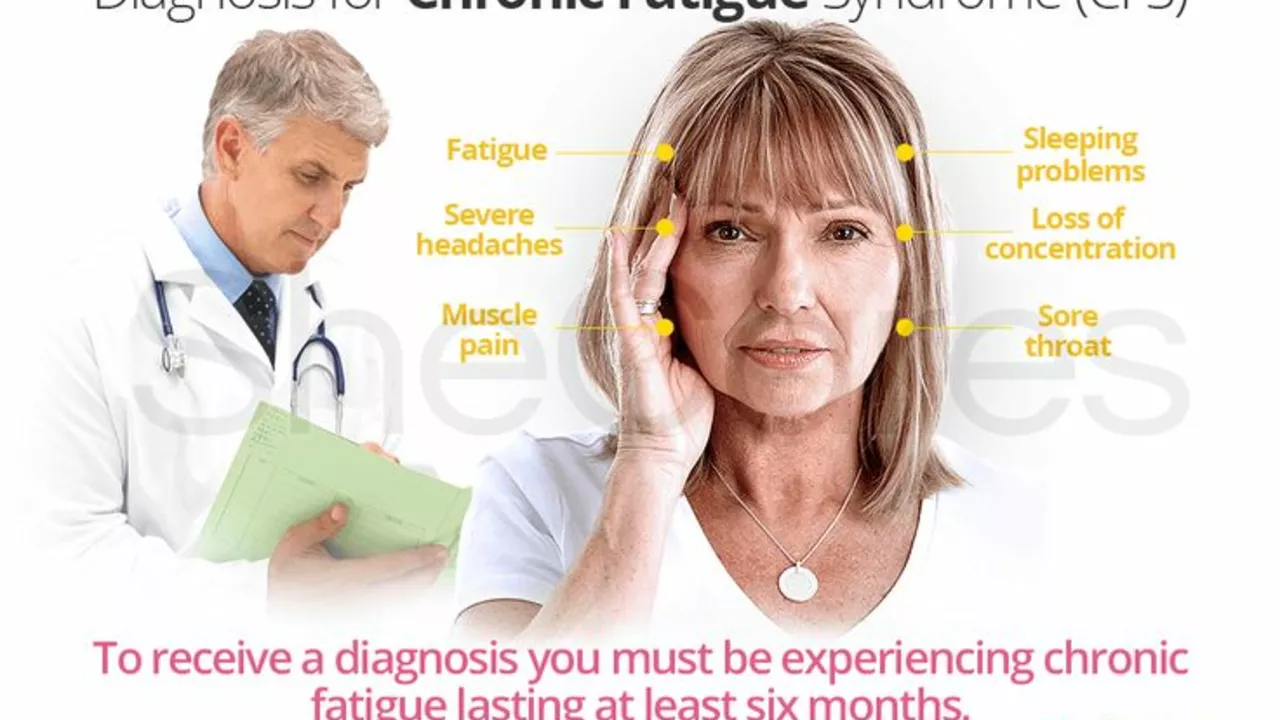
Quick signs, tests, and diagnosis
ME/CFS usually shows up as: severe fatigue that lasts 6+ months, PEM (worse symptoms after activity), unrefreshing sleep, cognitive issues ("brain fog"), and often orthostatic intolerance (feeling lightheaded when standing).
Doctors diagnose ME/CFS by ruling out other causes. Basic tests often include blood work (CBC, thyroid, liver, kidney, glucose), sleep study if sleep apnea is suspected, and orthostatic testing for POTS. Keep a symptom diary for 2–4 weeks before your visit—note activity, sleep, pain, and PEM triggers. That record makes the evaluation faster and more useful.
Practical daily strategies that actually help
Pacing beats pushing through. Learn your energy envelope: identify a safe daily activity level that avoids crashes, then stick close to it. Use timers and short rest breaks. Break tasks into tiny steps. For example, split a 20-minute walk into two 10-minute walks with a rest in between.
Manage orthostatic symptoms: drink more fluids, add salt if your doctor agrees, wear compression socks, and stand up slowly. Sleep hygiene helps—consistent sleep and wake times, reduce screens before bed, and short daytime naps (20–30 minutes) rather than long sleeps that worsen nighttime sleep.
Address specific symptoms with your healthcare team. For pain or sleep problems, low-dose medications or sleep aids may help. For brain fog, simple tools—lists, phone reminders, and one-task work—reduce mistakes and stress. If mood issues show up, therapy or a talk with your doctor can help; depression and anxiety are treatable and common alongside ME/CFS.
Be cautious with graded exercise therapy. Some people saw benefit, but many with PEM got worse. Talk to a clinician who understands ME/CFS before starting any activity program. A tailored, paced physical plan under guidance is safer than a fixed exercise prescription.
Want quick wins? Track symptoms, prioritize tasks, schedule hard activities for your best hours, and accept help without guilt. Ask your doctor for a clear plan and paperwork if you need work accommodations or disability support.
If symptoms are severe, suddenly worse, or you have concerning new signs (high fever, severe chest pain, new weakness), seek urgent care. For most people, careful pacing, symptom-focused care, and small daily changes make life steadier—and give you control back, step by step.