Physical Therapy for Joint Disorders: Improve Range of Motion and Build Strength
 Dec, 1 2025
Dec, 1 2025
When your knees ache getting out of bed, or your hips stiffen up after sitting too long, it’s not just aging-it’s your joints asking for help. Physical therapy isn’t a last resort for people who’ve tried everything else. It’s the most effective, science-backed way to regain movement and reduce pain in joint disorders like osteoarthritis and rheumatoid arthritis. And it works better than you might think.
Why Movement Is Medicine
For decades, the go-to fix for joint pain was rest, painkillers, or surgery. But that’s changing. The American College of Rheumatology updated its guidelines in 2021 to say something bold: exercise is disease-modifying therapy. That means moving your joints isn’t just helping you feel better-it’s actually slowing down damage. Studies show people who stick with their physical therapy routine have 23% slower joint degeneration over time compared to those who don’t.It’s not magic. It’s physics and biology. When you move, your joints produce synovial fluid-the natural lubricant that keeps cartilage healthy. Without movement, that fluid dries up. Cartilage starves. Pain gets worse. Physical therapy brings that fluid back.
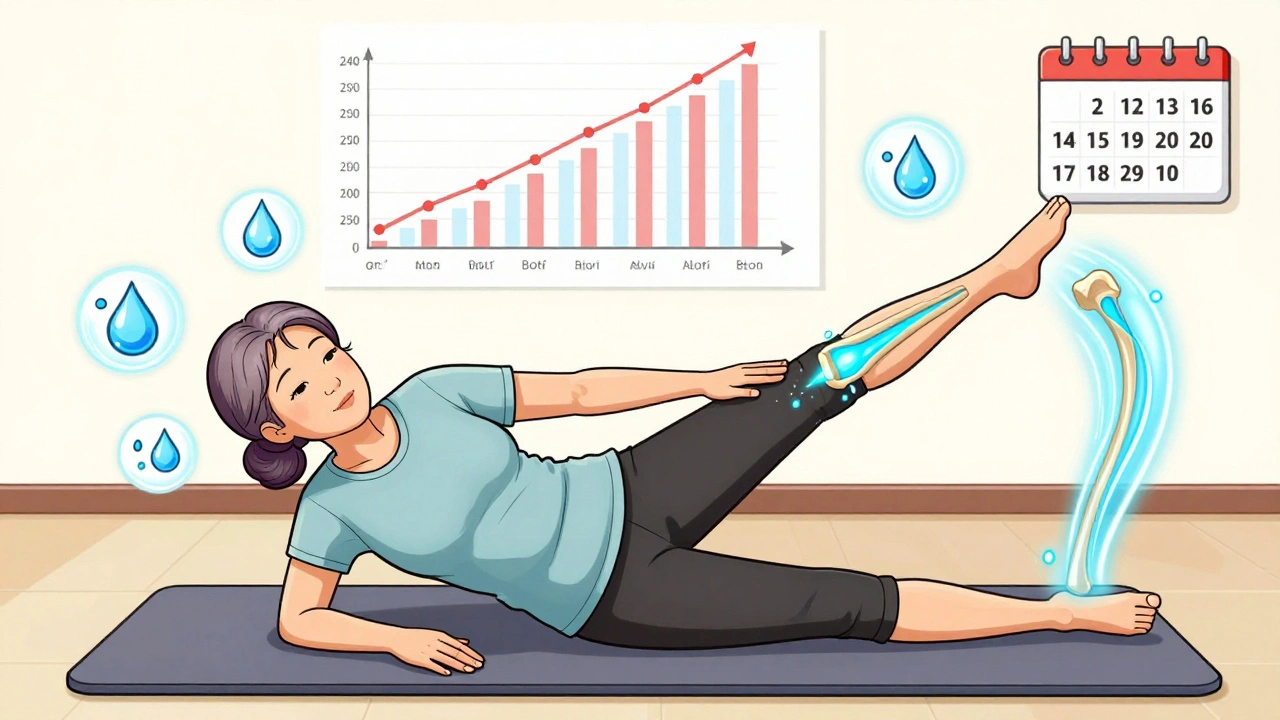
Range of Motion: The Foundation
Before you can strengthen a joint, you need to move it. That’s where range of motion (ROM) exercises come in. These aren’t fancy stretches. They’re precise, controlled movements designed to restore the natural arc your joint should move through.For knee osteoarthritis, therapists often start with terminal knee extension-gently straightening the knee from a bent position. You do this with a small ankle weight, usually 2.5 kg, for 3 sets of 10 to 15 reps, five days a week. The key? Keep pain under 3 out of 10. If it hurts more than that, you’re pushing too hard.
For hips, it’s hip flexion and abduction drills. You lie on your side and lift your leg slowly, keeping your pelvis stable. No swinging. No momentum. Just control. These movements aren’t meant to burn. They’re meant to retrain your brain to use the joint properly again.
And yes, it feels awkward at first. Your body has forgotten how to move correctly. But after 2 to 3 weeks, you’ll notice simple things change: you can stand up from a chair without using your hands. You can climb stairs without gripping the railing.
Strengthening: The Real Game-Changer
Once you’ve got some movement back, it’s time to build strength. But not just any strength. The right kind. For hip osteoarthritis, research recommends resistance training at 2.5 to 5.0 kg for 3 sets of 15 reps, three times a week. That’s not heavy. But it’s consistent.Why does this matter? Stronger muscles around the joint act like shock absorbers. They take pressure off the worn-out cartilage. A 2023 study in Arthritis & Rheumatology found that for mild-to-moderate hip OA, physical therapy delivered the same functional results as total hip replacement-at 12 months. And it didn’t require surgery.
For knees, it’s all about the quadriceps and hamstrings. Exercises like seated leg extensions, step-ups, and mini-squats (no deep squats!) are standard. Resistance starts low-40% of your one-rep max-and increases slowly. You don’t need to lift heavy. You need to lift smart.
And here’s something most people don’t know: isometric holds (tightening muscles without moving the joint) are powerful in the early stages. Try squeezing your thigh muscle while sitting, holding for 5 seconds, then relaxing. Do 10 reps, three times a day. It builds strength without stressing the joint.
When Physical Therapy Beats Surgery
You’ve probably heard that surgery is the only real fix for bad joints. But the data says otherwise. For knee osteoarthritis, physical therapy as a first step saves $7,842 per quality-adjusted life year compared to getting a cortisone shot right away. Medicare data shows patients who do physical therapy before knee replacement have 22% lower total costs and shorter hospital stays.And the numbers get even more striking for sacroiliac joint pain. A 2022 meta-analysis found that physical therapy combined with manual manipulation reduced pain by 68% after a year. NSAIDs? Only 32%. The number of people you need to treat with therapy to get one person a major improvement? Just 2.8. That’s better than most medications.
Physical therapy doesn’t just delay surgery-it can prevent it. The Arthritis Foundation estimates that if everyone with joint disorders got proper therapy, we could avoid 185,000 joint replacements every year. That’s $9.2 billion in healthcare savings.
What Doesn’t Work
Not all therapy is created equal. A 2022 study found that generic exercise plans-like just telling someone to “walk more”-only help 12 to 15% of patients. But individualized programs? That number jumps to 65 to 70%.Why? Because joints aren’t all the same. A 70-year-old with severe knee OA needs different exercises than a 50-year-old with early-stage hip arthritis. Therapy must be tailored. Your therapist should measure your progress with tools like the HOOS (Hip Disability and Osteoarthritis Outcome Score) or KOOS. A change of 8 to 10 points on these scales is what doctors consider clinically meaningful.
Also, don’t expect miracles overnight. The first two weeks often feel worse. That’s normal. Your body is adjusting. But if pain stays above 5/10 after two weeks, or you’re swollen and hot, tell your therapist. You might need to adjust the load or technique.
What to Expect in Sessions
Most physical therapy for joint disorders follows three phases:- Acute phase (0-2 weeks): Focus on reducing pain and restoring basic movement. Think gentle ROM-no resistance, no strain. For knee stiffness, that might mean sitting and slowly bending the knee 0 to 30 degrees.
- Subacute phase (2-6 weeks): Introduce isometric and light resistance work. Start with 20-30% of your max effort. Think wall sits, heel slides, seated leg lifts.
- Functional phase (6+ weeks): Progress to dynamic strengthening at 60-80% of your max. This is where you start walking uphill, doing step-ups, and eventually returning to daily activities without pain.
A typical course lasts about 14.7 sessions for knee OA. But most people see real progress by session 12-if they’re doing their home exercises.

Barriers and Real-Life Challenges
The biggest problem? Access. In rural areas, there’s one physical therapist for every 4,800 people. In cities, it’s 1 per 1,200. Many patients quit because they can’t get there-especially older adults without cars.Insurance limits are another hurdle. A 2023 survey found 58% of negative reviews on Yelp mention session caps. Some plans only cover 10 visits, even though 14-16 are often needed.
That’s why telehealth is growing fast. Starting in January 2025, Medicare and private insurers began reimbursing for remote physical therapy using wearable sensors that track your movement accuracy. If the device confirms you’re doing the exercise right, you get credit for the session.
And here’s a game-changer: neuromuscular electrical stimulation (NMES). A 2024 University of Pittsburgh study found that adding NMES to exercise boosted strength gains by 41% in knee OA patients after 24 weeks. It’s not magic. It’s a small device that gently shocks your muscle to make it contract. Your therapist can teach you how to use it at home.
How to Get Started
You don’t need a referral in every state, but most insurance plans require one. Talk to your doctor. Ask: “Can you refer me to a physical therapist who specializes in joint disorders?”Look for a therapist with:
- At least 120 hours of specialized musculoskeletal training
- Experience with OA or RA
- Use of validated outcome tools (HOOS, KOOS, DASH)
- A plan that includes home exercises and progress tracking
Don’t settle for a clinic that just gives you a generic handout. You deserve a plan built for your body.
What Success Looks Like
Real success isn’t about lifting heavy weights. It’s about doing the things you stopped doing:- Getting out of the car without groaning
- Walking to the mailbox without stopping
- Playing with your grandkids without pain the next day
- Sleeping through the night
On Healthgrades, physical therapy for joint disorders has a 4.2 out of 5 rating. 68% of patients report significant improvement in daily function within 8 weeks. That’s not hype. That’s data.
And if you’re wondering whether it’s worth the effort? Think of it this way: every hour you spend in therapy might buy you two extra years of pain-free movement. That’s not just treatment. That’s freedom.
Can physical therapy really replace surgery for joint pain?
For mild to moderate osteoarthritis, yes. Studies show physical therapy can deliver the same functional improvement as hip or knee replacement after 12 months. It won’t fix a bone-on-bone joint, but for most people, it delays or even prevents surgery. One study found patients who did therapy first postponed surgery by an average of 2.7 years.
How often should I do my exercises at home?
Consistency matters more than intensity. Most programs require 5 days a week of range of motion work and 3 days of strengthening. Missing a day isn’t the end, but if you skip more than 3 days a week, you’ll lose progress. Aim for at least 70% adherence-that’s the minimum threshold for noticeable benefit.
Why does my joint hurt more at first during therapy?
It’s common. When you start moving a stiff joint, you’re activating muscles that have been dormant and stressing tissues that have adapted to being still. This can cause temporary soreness. But it should never be sharp or last more than 24 hours. If pain stays above 3/10 or swells, tell your therapist. You might need to reduce resistance or change the exercise.
Is aquatic therapy better than land-based therapy?
It’s not better-it’s different. Water reduces joint load, making it ideal for people with severe pain or obesity. Sessions in 33-36°C water, 3 times a week, improve mobility with less discomfort. But land-based therapy builds strength more effectively for daily tasks. Many therapists combine both: water for early pain relief, land for functional gains.
How do I know if my physical therapy is working?
Ask for your baseline scores on tools like the HOOS or KOOS. A 10-point improvement means you’ve reached a clinically meaningful change. You should also notice daily improvements: climbing stairs without help, walking farther, sleeping through the night. If you’re not seeing these changes by week 6, ask your therapist to reassess your plan.
Can I do physical therapy on my own without a therapist?
You can start with basic movements, but you risk doing them wrong. A 2024 study found 63% of therapists prescribe different exercises for the same knee OA case. Without proper assessment, you might strengthen the wrong muscles or overload the joint. A single evaluation by a licensed therapist ensures you’re on the right track. After that, you can continue at home with supervision via telehealth.

Ella van Rij
December 2, 2025 AT 13:34sooo... you're telling me moving my knee doesn't require a PhD and a $2000 wearable sensor? i'm just gonna go do the heel slides now. thanks for the handout, doctor.
Zed theMartian
December 3, 2025 AT 19:56Oh please. Physical therapy? That’s what they give you when you can’t afford the real solution: a $50,000 robotic exoskeleton powered by quantum biofeedback. I’ve seen patients in Zurich who use AI-driven gait analysis with real-time synovial fluid viscosity mapping. You’re telling me lifting 2.5kg with a ‘3 out of 10 pain scale’ is science? That’s 1998 medicine. I weep for the future.
Also, the Arthritis Foundation? Please. They’re funded by Big Joint. Wake up.
ATUL BHARDWAJ
December 4, 2025 AT 14:00In India we have no PT clinics. We use yoga. We use coconut oil. We use patience. Sometimes it works. Sometimes it doesn't. But we don't need sensors or 14 sessions. We have our bodies. We have our time.
Steve World Shopping
December 5, 2025 AT 11:44Let me decode this for the layperson: You're advocating for low-load, high-frequency neuromuscular re-education protocols with progressive resistance paradigms to modulate nociceptive input and enhance proprioceptive feedback loops. In layman’s terms? Move slowly. Don’t overdo it. And stop Googling ‘knee pain cure’ at 3 AM.
Also, NMES? That’s just TENS with a fancy name. And no, your grandma’s heating pad isn’t ‘evidence-based.’
Rebecca M.
December 7, 2025 AT 09:17Ugh. I just spent 6 months doing this. My therapist cried when I told her I was quitting. Not because she was sad-because she knew I’d be back in a year with a knee brace and a lawsuit against my insurance. I’m not a patient. I’m a cautionary tale wrapped in compression sleeves.
Lynn Steiner
December 9, 2025 AT 02:45They took away my 20 visits. TWENTY. I needed 16. I got 12. Now my hip screams every time I pee. I'm not mad. I'm just... so tired. 😔
Alicia Marks
December 10, 2025 AT 22:08You got this. Even if it’s just 5 minutes a day. Tiny movements add up. You don’t have to be perfect-just consistent. And if you miss a day? Start again tomorrow. No guilt. Just movement.
Paul Keller
December 11, 2025 AT 09:08While the empirical data presented in this piece is statistically robust and aligns with contemporary clinical guidelines from the American College of Rheumatology, one must also consider the socioeconomic stratification inherent in healthcare delivery. The assertion that physical therapy can prevent 185,000 joint replacements annually presupposes universal access, equitable insurance coverage, and therapist availability-conditions demonstrably absent in rural America and among low-income populations. Furthermore, the reliance on outcome tools such as KOOS and HOOS, while valid, introduces measurement bias through self-reporting and cultural variance in pain perception. The integration of telehealth and NMES represents a promising frontier, yet without standardized protocols and regulatory oversight, these innovations risk becoming commodified solutions for the digitally privileged, exacerbating rather than mitigating disparities in musculoskeletal care.
Shannara Jenkins
December 11, 2025 AT 23:48Love this breakdown. Seriously. I’ve been doing the seated leg extensions and isometric quads for 3 weeks now. Last night, I got up from the couch without using my hands. I cried. Not because it was easy-but because I remembered what it felt like to move without fear. Keep going. You’re not broken. You’re rebuilding.