Chronic Kidney Disease Diet: What to Eat, Avoid, and Why It Matters
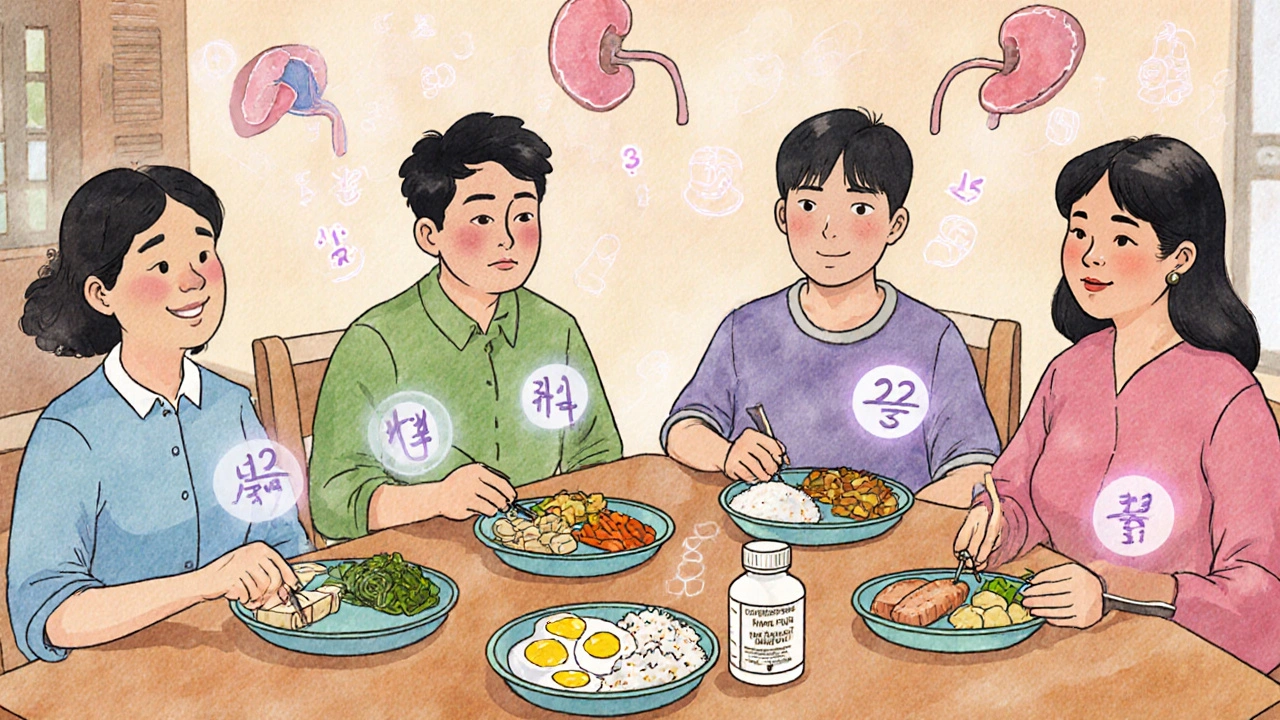
When your kidneys aren’t working right, what you eat becomes just as important as any medication. A chronic kidney disease diet, a personalized eating plan designed to reduce waste buildup and ease kidney strain. Also known as a renal diet, it’s not about starving yourself—it’s about choosing foods that help your body function without overloading damaged kidneys. This isn’t a one-size-fits-all plan. If your kidneys are struggling, they can’t filter out extra potassium, phosphorus, or sodium like they used to. That means even healthy foods like bananas, dairy, or canned soups can turn into hidden dangers.
That’s where low potassium diet, a key part of managing kidney disease to prevent dangerous heart rhythms comes in. High potassium can cause your heart to beat irregularly—or even stop. Foods like potatoes, spinach, oranges, and tomatoes often need to be limited or prepared in special ways, like leaching to pull out potassium. Then there’s low phosphorus diet, a strategy to stop calcium loss from bones and prevent dangerous calcifications in blood vessels. Processed foods, colas, and even some dairy products are packed with hidden phosphorus additives that your kidneys can’t clear. You’ll need to swap regular cheese for low-phosphorus options, choose fresh meats over processed ones, and read labels like a detective.
And sodium? It’s not just about high blood pressure. Too much salt makes your body hold onto water, which can lead to swelling, shortness of breath, and higher pressure on your heart. Salt substitutes? They’re often loaded with potassium—so skip them. Instead, use herbs, lemon juice, or vinegar to flavor meals. Fluid intake matters too. If you’re on dialysis, drinking too much between sessions can make you feel sick and increase your risk of heart strain. It’s not about drinking less for the sake of it—it’s about matching your intake to what your kidneys can handle.
What you’ll find in the posts below isn’t theory. It’s real-world advice from people who’ve lived with this. You’ll see how a chronic kidney disease diet connects to medications like those that manage potassium levels, how it overlaps with conditions like high blood pressure and diabetes, and how small changes—like choosing rice over potatoes or swapping soda for water—add up over time. There’s no magic bullet, but there are clear, doable steps that make a difference. Whether you’re newly diagnosed or managing this for years, the right food choices give you more control, fewer hospital visits, and better days.