Theophylline Clearance: How Common Medications Can Trigger Dangerous Toxicity
 Jan, 20 2026
Jan, 20 2026
Theophylline Clearance Risk Calculator
How Medications Affect Your Theophylline Levels
This calculator shows how other medications might increase your theophylline blood levels based on their clearance reduction effects. Theophylline has a narrow therapeutic range (10-20 mcg/mL). Levels above 20 can cause dangerous toxicity.
Your Estimated Theophylline Level
Recommendations
When you take theophylline for asthma or COPD, even a small change in your other medications can push your blood levels into the danger zone. It’s not just about taking more pills-it’s about how those pills change the way your body processes theophylline. The difference between safe and life-threatening can be as little as a 10% drop in clearance. And many people don’t even know it’s happening until they end up in the ER.
Why Theophylline Is So Fragile
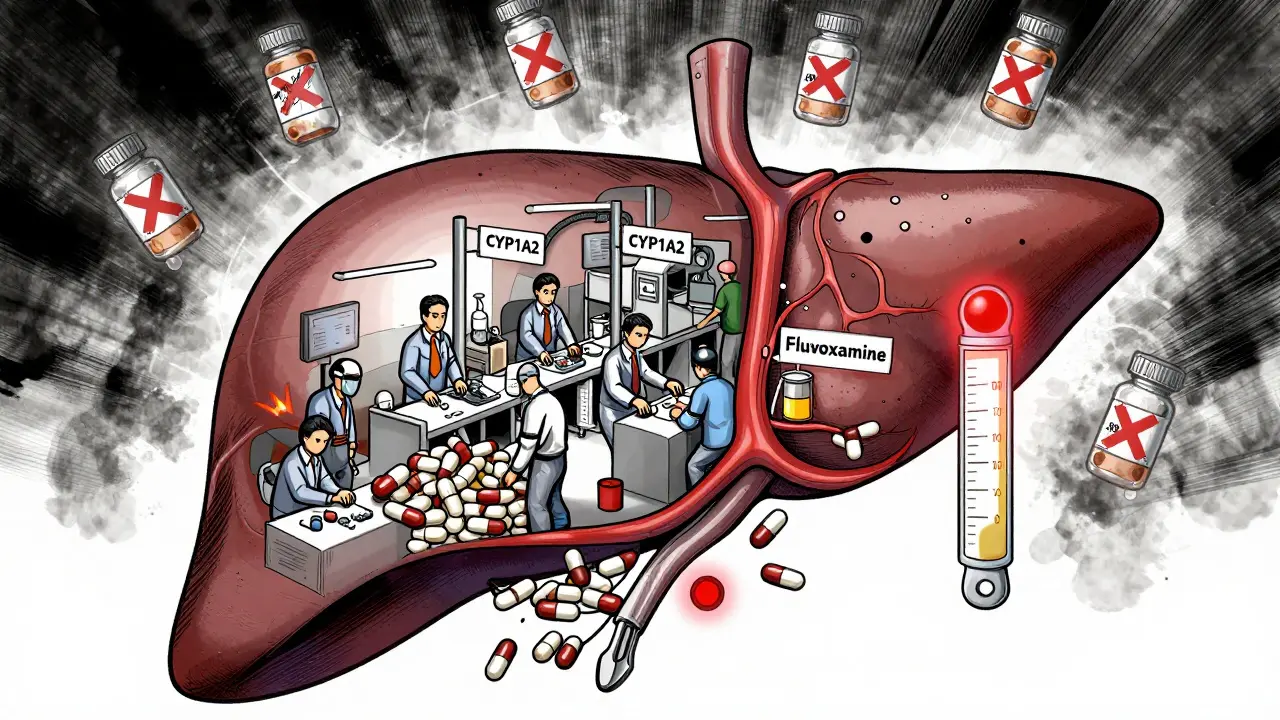
Theophylline isn’t like most asthma meds. It doesn’t just relax your airways-it works deep inside your cells. But here’s the catch: your body breaks it down fast, and that breakdown is easily disrupted. About 90% of theophylline is processed by your liver using an enzyme called CYP1A2. This enzyme is picky. It’s sensitive to other drugs, even ones you’d never think could interfere.
And the margin for error? Tiny. The safe range is 10 to 20 micrograms per milliliter. Go above 20, and you risk nausea, vomiting, rapid heartbeat, seizures-even death. Go below 10, and your asthma isn’t controlled. That’s why doctors used to check blood levels every few weeks. Many still do, especially in older adults or people on multiple medications.
What makes it worse? Theophylline doesn’t follow normal rules. At therapeutic doses, its metabolism becomes nonlinear. That means a small increase in dose-or a small drop in clearance-can cause a huge spike in blood levels. One study showed that when clearance drops by just 20%, serum levels can jump 50% or more. That’s not a linear relationship. It’s a cliff edge.
Top Medications That Slow Down Theophylline Clearance
Not all drugs affect theophylline the same way. Some barely move the needle. Others are outright dangerous. Here are the biggest culprits, ranked by how much they reduce clearance:
- Fluvoxamine (an SSRI antidepressant): Reduces clearance by 40-50%. This is the most dangerous interaction. The European Respiratory Society says to avoid combining them entirely. A 2021 study found patients on both had a 12.7 times higher risk of toxicity.
- Cimetidine (an old-school heartburn drug): Drops clearance by 25-30%. Still used in some places because it’s cheap. But if you’re on theophylline and start taking Tagamet, your levels can rise from 15 to over 25 mcg/mL in under 72 hours. That’s toxic territory.
- Allopurinol (for gout): Reduces clearance by 20%. Many assume it’s harmless because it’s used for gout. But in a 1984 study, patients on 600 mg of allopurinol daily needed a 20% theophylline dose reduction. Even lower doses can matter if you’re already near the top of the safe range.
- Erythromycin and Clarithromycin (antibiotics): Cut clearance by 15-25%. These are common for chest infections. If you’re on theophylline and get pneumonia, your doctor might prescribe one of these-without realizing the risk.
- Furosemide (a water pill): Some studies show a 10-15% drop in clearance. Others show no effect. But in older patients with heart failure, even a small change can tip the balance.
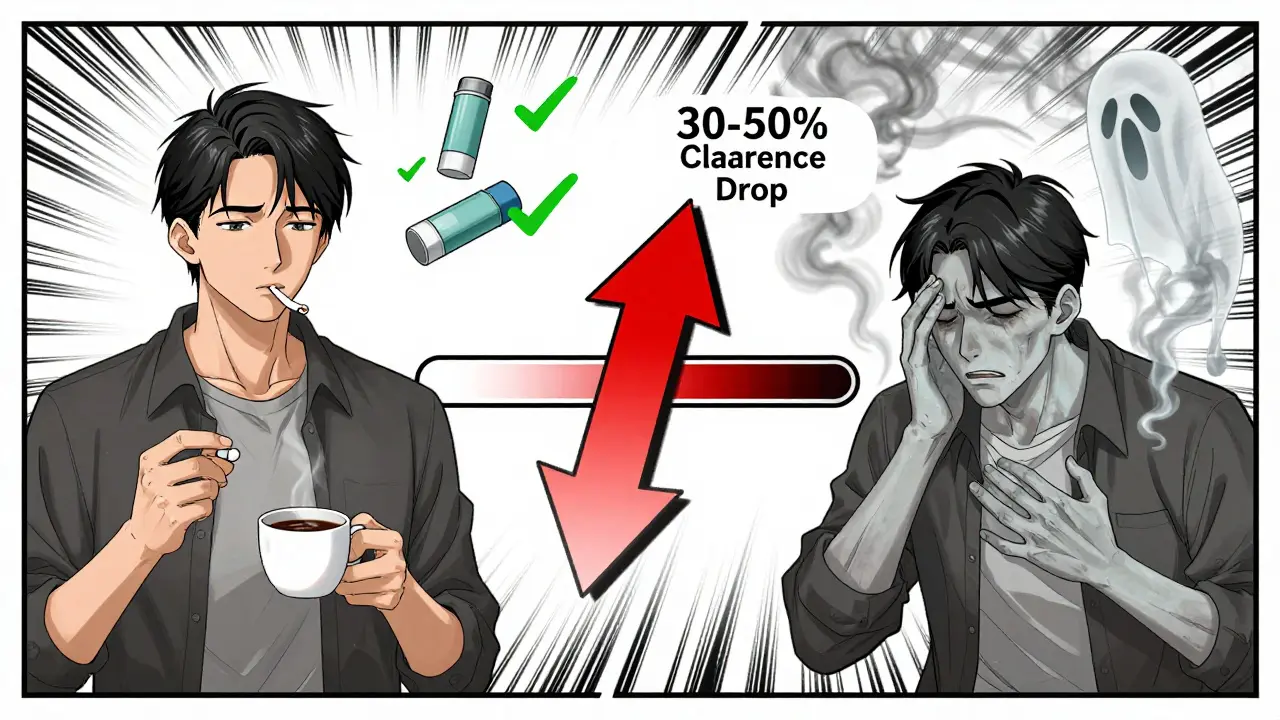
And here’s something most people miss: smoking cessation. If you’ve been smoking for years and suddenly quit, your CYP1A2 enzyme activity drops by 30-50% within two weeks. That’s like adding a powerful inhibitor without taking a single pill. Combine that with starting cimetidine or fluvoxamine? You’re asking for trouble.
What Happens When Clearance Drops
Imagine your body is a factory. Theophylline is the product. CYP1A2 is the assembly line. Normally, the line runs smoothly, processing 3 liters of the drug per hour in a healthy adult. Now, someone throws a wrench into the gears. The line slows down. Products pile up. The factory overflows.
That’s what happens in your liver. When CYP1A2 is blocked, theophylline builds up. Symptoms start subtly: headache, jitteriness, upset stomach. Then come the red flags-palpitations, tremors, confusion. Seizures and arrhythmias follow. In one case documented in Respiratory Medicine, a 72-year-old man on stable theophylline (15.2 mcg/mL) started cimetidine for acid reflux. Three days later, his level was 24.7 mcg/mL. He had atrial fibrillation and was hospitalized.
These aren’t rare. In 2022, the FDA recorded 1,842 theophylline-related adverse events in the U.S. Over 40% were due to drug interactions. And that’s just the ones reported. Many more go unreported, especially in nursing homes or rural clinics where blood monitoring isn’t routine.
Who’s at Highest Risk?
It’s not just about the drugs. It’s about who’s taking them.
- Older adults: Liver function declines with age. Clearance drops naturally. One study found elderly patients with heart failure clear theophylline at less than one-third the rate of healthy young adults.
- People with COPD: Often on multiple meds-antibiotics, diuretics, heart meds, painkillers. Polypharmacy is the norm, not the exception.
- Patients with liver disease: Even mild cirrhosis cuts clearance by 40%.
- Non-smokers: Smoking boosts CYP1A2. Quitting removes that boost. Many patients don’t tell their doctors they stopped smoking.
A 2021 study of 1,247 patients over 65 found that nearly 3 out of 10 were on a drug that reduced theophylline clearance. Only 37% had their dose adjusted. That’s a recipe for disaster.
How to Stay Safe
If you’re on theophylline, here’s what you need to do:
- Know your meds. Keep a list of everything you take-including over-the-counter drugs, herbal supplements, and antacids. Cimetidine is in some cold and pain meds. Fluvoxamine is in Luvox and some generics.
- Ask before starting anything new. Even if it’s just a new painkiller or heartburn pill. Say: “I’m on theophylline. Is this safe?”
- Get your blood tested. If you start or stop any of the drugs listed above, ask for a serum theophylline level within 48-72 hours. The American Association for Clinical Chemistry says this is standard care.
- Watch for symptoms. Nausea, fast heartbeat, shaking, confusion? Don’t wait. Call your doctor. Don’t assume it’s just a bug or stress.
- Don’t quit smoking cold turkey without telling your doctor. If you stop smoking, your theophylline dose may need to be lowered by 30-50%.
Some hospitals now use electronic alerts to flag these interactions. But a 2023 survey of 412 pulmonologists found that 62% said their EHR systems didn’t warn them about theophylline interactions often enough. You can’t rely on technology alone.
What About Newer Alternatives?
Yes, newer bronchodilators like salmeterol, formoterol, and tiotropium are safer and more predictable. They don’t need blood tests. They don’t interact with half your medicine cabinet. That’s why theophylline use has dropped by 62% in the U.S. since 2000.
But it’s not gone. In places where newer drugs are expensive or unavailable, theophylline is still a lifeline. It’s also used for severe nocturnal asthma that doesn’t respond to other treatments. And now, researchers are testing very low doses (100-200 mg daily) for its anti-inflammatory effects in COPD. But these trials exclude anyone on CYP1A2 inhibitors-because the risk is too high.
The bottom line? Theophylline isn’t obsolete. But it’s a high-risk tool. And like a chainsaw, it needs respect.
When to Call It Quits
If you’re on long-term cimetidine, fluvoxamine, or allopurinol, your doctor should consider switching you off theophylline entirely. The NICE guidelines in the UK say to avoid combining them. And with good reason: a 2023 audit found 92% of UK respiratory specialists agree.
There’s no shame in switching to a safer drug. If you’ve been stable on theophylline for years but now need an antidepressant or gout treatment, talk to your doctor about alternatives. There are options. Theophylline doesn’t have to be your only choice.
It’s not about being old-fashioned. It’s about staying alive.
Can I take ibuprofen with theophylline?
Yes, ibuprofen doesn’t significantly affect theophylline clearance. Most NSAIDs like naproxen and celecoxib are safe. But avoid aspirin in high doses-it can slightly increase theophylline levels. Always check with your doctor if you’re on high-dose or long-term NSAIDs.
Does caffeine interact with theophylline?
Caffeine is chemically similar to theophylline and is metabolized by the same enzyme, CYP1A2. Drinking large amounts of coffee, energy drinks, or tea can compete for metabolism and slightly raise theophylline levels. If you’re on theophylline, limit caffeine to 1-2 cups of coffee per day. Sudden caffeine reduction can also raise levels-so don’t quit cold turkey.
What if I accidentally took cimetidine with theophylline?
Stop the cimetidine immediately and contact your doctor. Don’t wait for symptoms. Ask for a serum theophylline level within 24-48 hours. If your level is above 20 mcg/mL, you may need IV fluids, activated charcoal, or even dialysis in severe cases. Do not try to adjust your dose yourself.
Is theophylline still used today?
Yes, but only in specific cases. It’s still used for severe nocturnal asthma, COPD patients who can’t afford newer inhalers, and in low-resource settings. Global use has dropped sharply in North America and Europe, but it remains common in parts of Asia and Africa. New research is exploring very low doses for anti-inflammatory effects-but only in patients not taking interacting drugs.
How often should theophylline levels be checked?
When you first start, levels should be checked after 3-5 days. After that, check every 3-6 months if stable. But if you start or stop any medication, change your smoking habits, or develop liver problems, check within 48-72 hours. Many patients go years without a check-and that’s dangerous.

Kelly McRainey Moore
January 22, 2026 AT 07:24Wow, I had no idea smoking cessation could mess with theophylline like that. My grandma was on it for years and quit cold turkey last year-she ended up in the ER with a racing heart. No one told her it could be linked. This post should be mandatory reading for anyone over 50 on asthma meds.
Also, caffeine? I drink three espressos a day. Guess I’m cutting back now.
Amber Lane
January 23, 2026 AT 00:11My mom’s on theophylline and just started fluvoxamine for anxiety. Her doctor didn’t mention the interaction. She’s lucky she didn’t have a seizure. This needs to be screamed from the rooftops.
Ashok Sakra
January 24, 2026 AT 15:21THIS IS WHY AMERICA IS DYING. EVERYONE JUST TAKES PILLS LIKE CANDY. NOBODY THINKS. NOBODY CARES. YOUR LIVER IS NOT A TOY. I TOLD YOU THIS. I TOLD YOU ALL.
THEY PUT THIS DRUG ON THE MARKET IN 1950S AND STILL LET PEOPLE USE IT???
lokesh prasanth
January 25, 2026 AT 08:35theophylline is just a reminder that pharma never really fixed the root problem. they just made new pills to cover up the old ones breaking. we need better lungs not better chemistry.
Samuel Mendoza
January 25, 2026 AT 14:24So you’re telling me a 70-year-old on three meds and a pacemaker shouldn’t be on theophylline? Shocking. I guess the FDA just forgot to update the 1980s guidelines. Maybe if people stopped being lazy and exercised, they wouldn’t need any of this.
shubham rathee
January 27, 2026 AT 05:18you know what else blocks CYP1A2? 5G towers and the government's secret fluoride in the water. i bet they dont tell you that. they want you dependent on theophylline so they can sell you more pills. i saw a video on tiktok where a guy cured his asthma with turmeric and a crystal. i think we need to go back to nature.
MAHENDRA MEGHWAL
January 28, 2026 AT 15:24Thank you for this meticulously detailed and clinically accurate exposition. The metabolic kinetics described are precisely aligned with current hepatobiliary pharmacology literature. I shall share this with my geriatric ward colleagues. A rare instance of clarity in an age of noise.
Kevin Narvaes
January 28, 2026 AT 17:06so like… the body’s a factory? and the liver’s the assembly line? and theophylline’s the product? bro that’s literally the metaphor from that one med school video i watched in 2017. i still remember the guy with the whiteboard. we were all like ‘yo this is wild’ and then i forgot everything until now. thanks for the nostalgia trip.
Sangeeta Isaac
January 29, 2026 AT 02:37so let me get this straight… i can’t have my morning coffee AND my allopurinol AND my new antidepressant AND my asthma pill without turning into a human seizure machine? cool cool cool. just another day in the glorious future of medicine where we’re all just one bad decision away from the ICU.
also, why is this not a pop-up warning on every pharmacy app? someone get a grant.
Ben McKibbin
January 29, 2026 AT 09:16This is one of the most important public health posts I’ve read in years. Theophylline isn’t outdated-it’s misunderstood. We need mandatory pharmacist counseling when it’s prescribed, not just a footnote in the drug leaflet. And yes, smoking cessation absolutely needs to be flagged as a drug interaction. That’s not common sense, that’s medical negligence.
Also, to the guy who said ‘exercise more’-your comment is tone-deaf and dangerous. COPD isn’t caused by laziness. It’s caused by decades of pollution, poverty, and lack of access. Stop blaming patients. Fix the system.
Melanie Pearson
January 31, 2026 AT 01:08It is unacceptable that American healthcare permits such a precarious therapeutic regimen to persist in the 21st century. This is not medicine-it is pharmaceutical roulette. The fact that this drug remains in use while safer alternatives exist speaks volumes about the corruption and inefficiency of the U.S. healthcare industrial complex. We must abolish theophylline entirely and invest in universal access to bronchodilators. This is a moral failure.
Uju Megafu
January 31, 2026 AT 03:16Y’all in the US be scared of one little pill but in Nigeria we give our grandma theophylline with palm oil and pray. She still walking. You think your EHR system is smart? We got Auntie Mary with the WhatsApp group that knows every drug in the market. If you take cimetidine, she calls you. No algorithm. Just love. This post is good but you missed the real solution: community.