Chronic Kidney Disease: How Early Detection Stops Progression
 Jan, 7 2026
Jan, 7 2026
Chronic kidney disease doesn’t announce itself. No sharp pain. No fever. No obvious warning. By the time most people feel something is wrong, their kidneys are already failing. And yet, chronic kidney disease affects 1 in 7 American adults-nearly 37 million people-and more than half don’t know they have it. The good news? If caught early, you can stop it from getting worse. Not just slow it. Stop it. For many, that’s possible.
What Chronic Kidney Disease Really Means
Chronic kidney disease (CKD) isn’t one single illness. It’s a label for when your kidneys aren’t working the way they should-for at least three months. That doesn’t mean they’ve stopped. It means they’re struggling. Maybe they’re filtering too slowly. Maybe they’re leaking protein into your urine. Either way, the damage is real, and it’s progressive.
The kidneys don’t just make urine. They regulate blood pressure, balance electrolytes, remove waste, and even help make red blood cells. When they falter, everything else starts to slip. That’s why CKD is linked to heart disease, stroke, and early death-not just dialysis.
There are five stages of CKD, based on how well your kidneys filter blood. Stage 1 is mild damage with normal or near-normal function. Stage 5 is kidney failure. The goal isn’t to avoid Stage 5. The goal is to never get there. And that starts with two simple tests.
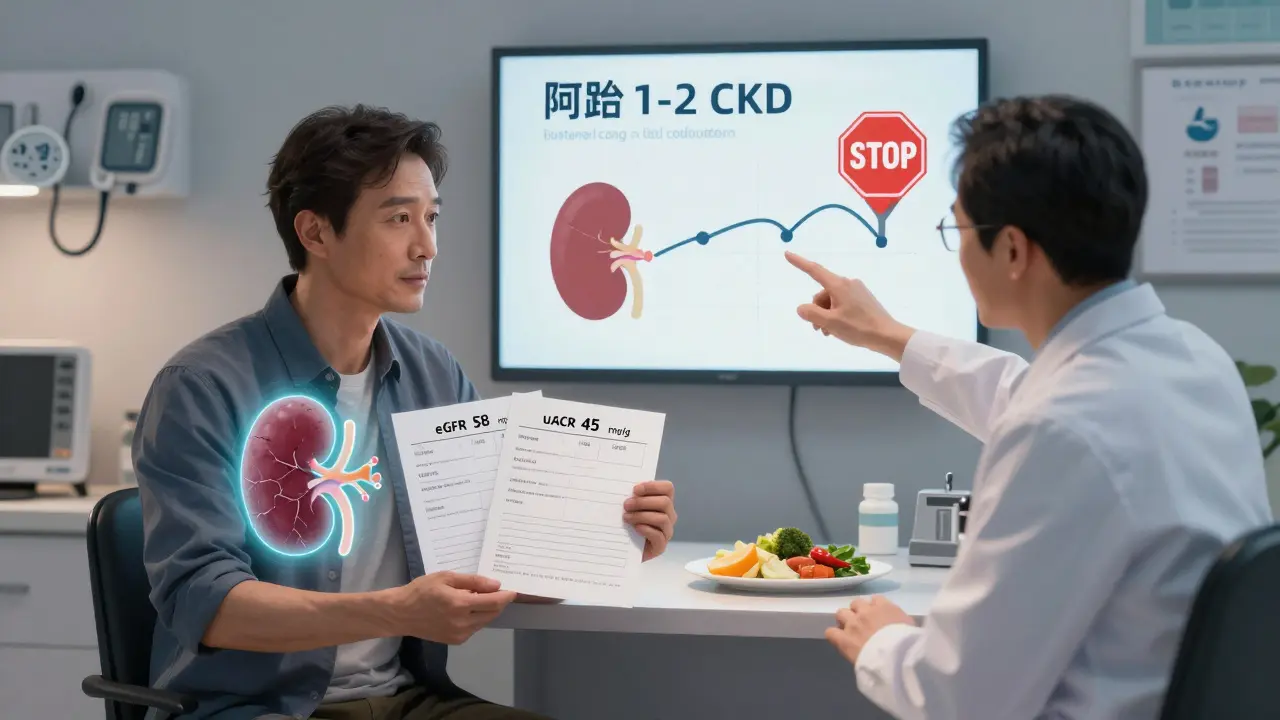
The Two Tests That Catch CKD Early
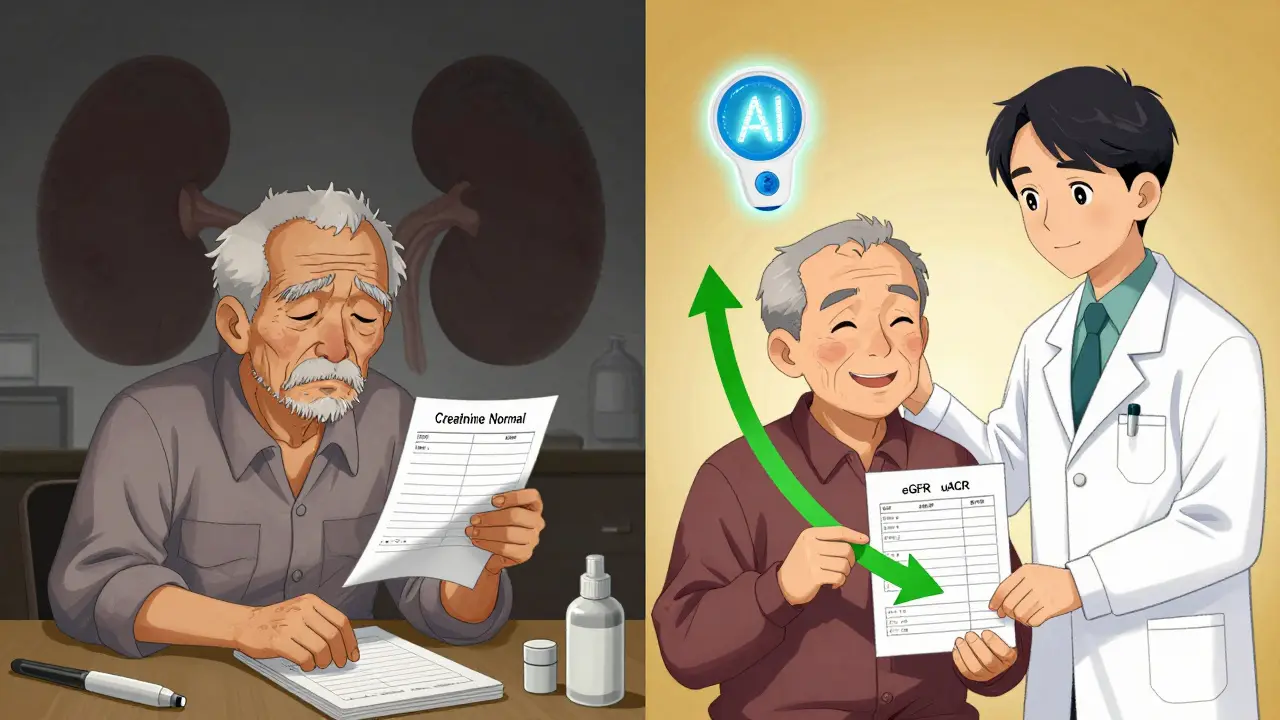
For decades, doctors checked one thing: serum creatinine. It’s cheap. It’s easy. And it misses nearly half of early kidney disease.
Today, guidelines from KDIGO and the National Kidney Foundation demand two tests-always together:
- eGFR (estimated glomerular filtration rate): This estimates how well your kidneys filter waste. It’s calculated from your blood creatinine, age, sex, and race. A value below 60 for three months or more signals CKD.
- uACR (urine albumin-to-creatinine ratio): This checks for protein in your urine. Healthy kidneys don’t let albumin escape. If your uACR is 30 mg/g or higher, your kidneys are leaking. That’s a red flag-even if your eGFR is normal.
Here’s the key: You can have normal eGFR and still have CKD if your uACR is high. That’s how early damage hides. And that’s why checking only creatinine is outdated. A 2018 study found that relying on creatinine alone missed 30-40% of early CKD cases.
For some people-especially older adults or those with low muscle mass-creatinine can be misleading. In those cases, doctors may check cystatin C, a more accurate marker of kidney function that isn’t affected by diet or muscle mass.
Who Should Be Screened-and How Often
CKD doesn’t pick favorites. But some people are at much higher risk.
- People with diabetes: The leading cause of CKD. Screen annually starting at diagnosis for Type 2, or five years after diagnosis for Type 1.
- People with high blood pressure: The second leading cause. Get tested at every visit, with full eGFR and uACR at least once a year.
- Those with a family history of kidney failure.
- African Americans, Native Americans, and Hispanic populations: These groups have 2-4 times higher risk. Don’t wait for symptoms.
- People over 60: Kidney function naturally declines with age, but that doesn’t mean damage is normal.
And if you’re on long-term NSAIDs like ibuprofen, or have autoimmune diseases like lupus? You’re at risk too.
Screening isn’t optional for these groups. It’s essential. And it’s cheap: about $30 a year per person. But skipping it can cost $1,850 per person in avoidable complications.
How Early Detection Actually Stops Progression
Most people think CKD is inevitable once it starts. It’s not.
Studies show that catching CKD in Stage 1 or 2 gives you a 5-7 year window to act. In 60-70% of cases, you can stop it from getting worse.
How? Three proven strategies:
- Control blood pressure: Aim for under 130/80. The SPRINT trial showed this cuts progression risk by 27% compared to the older target of 140/90.
- Use SGLT2 inhibitors: Originally diabetes drugs, these (like dapagliflozin and empagliflozin) now have FDA approval for CKD-even without diabetes. The CREDENCE trial showed they reduce progression to kidney failure by 32%.
- Reduce protein in your diet: Too much protein strains damaged kidneys. A registered dietitian can help you find the right balance-enough to stay strong, not so much that it accelerates damage.
One 2022 meta-analysis found that patients who got full early intervention-medication, diet, education-slowed their kidney decline from 3.5 mL/min/year to just 1.2 mL/min/year. That’s not just slowing. That’s nearly halting.
Why So Many Cases Are Still Missed
If the tests are simple and the benefits are clear, why are so many people still diagnosed late?
Because the system isn’t designed for early detection.
A 2022 study found that only 53% of primary care doctors consistently order both eGFR and uACR. In rural clinics, that number drops to under 32%. Why? Electronic health records rarely remind them. Many still think “normal creatinine” means “normal kidneys.”
Patients aren’t blameless either. A Reddit thread from 2023 had hundreds of stories like this: “My doctor checked creatinine for 10 years. When they finally did uACR, I was already Stage 3.”
But there’s hope. The Kidney Precision Medicine Project created standardized reporting templates that cut diagnostic errors by 35%. The National Kidney Foundation’s patient education materials improved understanding by 28% in just a few months. And now, the Biden administration is funding a $150 million push to make dual-testing mandatory in Federally Qualified Health Centers by 2026.
What’s Next: AI, Point-of-Care Tests, and Fairer Science
Technology is catching up.
In 2023, the FDA cleared the first AI tool-NephroSight by Renalytix-that analyzes 32 data points to predict who’s at risk of CKD before their eGFR drops. It’s being tested in VA hospitals and could soon be in primary care offices.
Point-of-care uACR tests are coming too. By 2025, you might get your urine protein result in 10 minutes during a routine visit-no lab wait, no delay.
And then there’s the race issue. For years, eGFR calculations added a “race correction” for Black patients, assuming they had more muscle mass. That meant their kidney function looked better than it was. Removing this bias could increase early detection in African Americans by over 12%. Major medical groups are now pushing to drop it entirely.
Your Next Steps
If you have diabetes, high blood pressure, or a family history of kidney disease:
- Ask your doctor for both eGFR and uACR-don’t accept creatinine alone.
- If you’re over 60, ask even if you feel fine.
- If your results are borderline (eGFR 45-59 or uACR 30-300), ask for a repeat test in 3 months. One abnormal result isn’t enough-both must be abnormal for three months to confirm CKD.
- If you’re diagnosed early, don’t panic. Work with your doctor on blood pressure control, ask about SGLT2 inhibitors, and see a dietitian.
CKD isn’t a death sentence. It’s a warning. And warnings are meant to be heeded.
Can chronic kidney disease be reversed?
Early-stage CKD (Stages 1-2) can often be stabilized or even improved with proper management. While existing scarring can’t be undone, further damage can be prevented. Many people with Stage 1 or 2 CKD live for decades without progression if they control blood pressure, manage diabetes, avoid NSAIDs, and follow dietary advice.
Is CKD the same as kidney failure?
No. Kidney failure is Stage 5 CKD, when the kidneys work at less than 15% of normal capacity. Most people with CKD never reach this stage. CKD is a spectrum-from mild damage to complete failure. Early detection keeps you far from failure.
Do I need a kidney biopsy if I have CKD?
Rarely. Most cases are diagnosed with blood and urine tests. A biopsy is only done if the cause is unclear after standard testing-like if you have blood in your urine without diabetes or high blood pressure, or if your kidneys are shrinking without a clear reason. It’s needed in fewer than 2% of cases.
Can I still drink alcohol with CKD?
Moderation is key. One drink a day for women, two for men, is generally safe if your blood pressure is controlled. But alcohol can raise blood pressure and interact with medications. If you’re unsure, ask your doctor. Many people with early CKD choose to cut back or quit-not because they have to, but because it helps.
Why do some doctors still only check creatinine?
Many haven’t updated their practice since the 2000s. Electronic health records don’t always prompt for both tests. Some still believe creatinine is enough. Others are overwhelmed by workload. But guidelines have changed. The two-test approach is now standard. If your doctor only orders creatinine, ask why-and ask for uACR too.
Are there any symptoms of early CKD?
Almost none. That’s why it’s called a silent disease. By the time you feel tired, swollen, or nauseous, your kidneys are already significantly damaged. Don’t wait for symptoms. If you’re at risk, get tested.
Can lifestyle changes really make a difference?
Yes. A 2022 study showed that patients who followed a kidney-friendly diet, exercised regularly, and took prescribed medications slowed their kidney decline by more than 65% compared to those who didn’t. It’s not magic-it’s consistency. Small changes, over time, add up to big results.
Final Thought: Don’t Wait for the Warning Signs
Chronic kidney disease is preventable-if you catch it early. The tools are here. The science is clear. The cost of waiting is too high-not just in dollars, but in life. If you’re at risk, ask for the two tests. If you’ve been told your kidneys are fine but your creatinine was the only test, ask again. You’re not being difficult. You’re being smart.

swati Thounaojam
January 7, 2026 AT 12:57my doc only checked creatinine for 5 years. when they finally did uacr, i was stage 3. why is this still a thing?
christy lianto
January 8, 2026 AT 17:47if you have diabetes or high bp, you’re already at war with your body. why are we still playing catch-up with basic tests? this isn’t rocket science-it’s basic care. stop waiting for symptoms. get the two tests. now.
Ken Porter
January 8, 2026 AT 18:36we’re spending billions on fancy ai tools while doctors still use 2005 protocols. america’s healthcare system is broken. fix the basics first.
Dave Old-Wolf
January 10, 2026 AT 06:13i never knew uacr was a thing. my dad had kidney issues but they only ever checked his blood. he ended up on dialysis at 62. if we’d known earlier…
so if your eGFR is fine but uacr is high, you still have kidney damage? that’s wild. why isn’t this taught in med school?
Kristina Felixita
January 12, 2026 AT 00:55my cousin got diagnosed with stage 2 last year-she’s 48, diabetic, and had zero symptoms. her doctor finally ordered the uacr after she begged. now she’s on an SGLT2 inhibitor, lost 15 lbs, and her numbers are improving. it’s not magic-it’s just doing the right thing.
if you’re at risk, don’t wait for a miracle. ask for the test. say it twice. say it louder.
you’re not being annoying-you’re being alive.
Joanna Brancewicz
January 12, 2026 AT 16:56the race correction in eGFR was a structural bias disguised as clinical science. removing it increases early detection in Black patients by 12%. this isn’t politics-it’s biostatistics. why did it take this long?
Evan Smith
January 12, 2026 AT 22:03so let me get this straight… we have a $150 million federal push to fix a test that should’ve been standard in 2010? and we’re only doing it now because someone finally said "wait, this is ridiculous"?
brilliant. just brilliant.
Lois Li
January 14, 2026 AT 04:43i work in a rural clinic. we get maybe 20 patients a day. the EHR doesn’t auto-populate uACR. no reminders. no templates. no training. we do what we can with what we’ve got.
but i’ve started printing out the KDIGO guidelines and handing them to patients. some of them go home and ask their docs for the test. it’s small, but it’s something.
we’re not failing them-we’re just under-resourced. and that’s the real problem.
Aubrey Mallory
January 15, 2026 AT 06:47if your doctor only checks creatinine, they’re not just outdated-they’re negligent. this isn’t a suggestion. it’s medical malpractice waiting to happen. i’ve seen people die because they trusted a single number. don’t be one of them.
Donny Airlangga
January 17, 2026 AT 06:13my mom’s got stage 2 CKD. she’s 71. no symptoms. just tired. we asked for the uACR because of this post. turns out her protein levels were sky-high. she’s on meds now, eating better, and feels better than she has in years.
the takeaway? if you’re over 60, even if you feel fine, ask for both tests. it’s not scary. it’s just smart.