Diabetic Kidney Disease: How Early Albuminuria Signals Risk and Why Tight Control Saves Kidneys
 Dec, 31 2025
Dec, 31 2025
When your kidneys start leaking protein, it’s not just a lab result-it’s your body screaming for help. In people with diabetes, the earliest warning sign of kidney damage isn’t swelling, fatigue, or high blood pressure. It’s something invisible: albuminuria. This tiny amount of protein in the urine is the first red flag that diabetic kidney disease (DKD) is taking root. And here’s the truth: catching it early and acting fast can stop it in its tracks.
What Is Albuminuria, Really?
Albumin is a protein your kidneys normally keep inside your blood. When they’re healthy, they don’t let it slip into your urine. But when high blood sugar damages the tiny filters in your kidneys, albumin starts leaking out. That’s albuminuria.
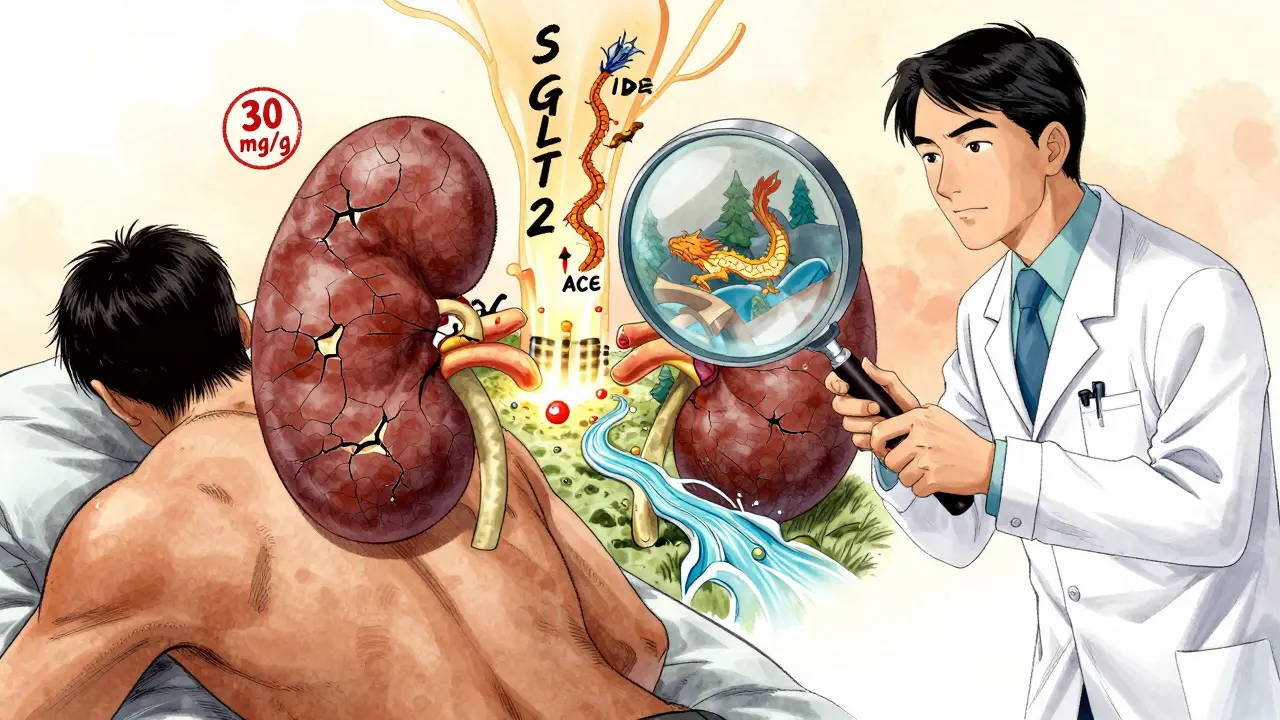
It’s not a single number. It’s a spectrum. The Urine Albumin-to-Creatinine Ratio (UACR) measures how much albumin is in your urine compared to creatinine, a waste product. The standard cutoffs? Less than 30 mg/g is normal. Between 30 and 300 mg/g? That’s moderately increased albuminuria-what doctors used to call microalbuminuria. Over 300 mg/g? Severely increased. And here’s the key: any albumin above 30 mg/g means your kidneys are already hurt.
That’s a shift from old thinking. In the past, doctors waited for big protein leaks before worrying. Now, we know even small leaks matter. A 2021 analysis of over 128,000 diabetic patients found that those with UACR above 300 mg/g had a 73% higher risk of dying from any cause-and an 81% higher risk of heart-related death-than those with no albumin in their urine.
Why Testing Isn’t Optional
Every person with type 2 diabetes should get a UACR test at diagnosis. For those with type 1 diabetes, it’s time to test after five years. That’s not a suggestion. It’s a Class A recommendation from the American Diabetes Association-the highest level of evidence. Yet, only 58% to 65% of clinics actually do it regularly.
Why the gap? Many patients don’t collect urine properly. Others get results back from a random test and panic, only to find out their UACR was high because they ran a 5K the day before, had a fever, or their blood sugar spiked past 300 mg/dL. These are temporary spikes. That’s why guidelines say: don’t diagnose based on one test. You need two abnormal results out of three, collected over 3 to 6 months.
Spot checks are the norm in clinics-just a single urine sample. But if you’re told your UACR is high, don’t assume the worst. Ask: “Was this tested under stable conditions?” If not, retest. Give your body time to reset.
Tight Control Isn’t Just About Sugar
The landmark DCCT/EDIC study changed everything. In type 1 diabetes, keeping HbA1c below 7% cut the risk of developing microalbuminuria by 39% and full-blown proteinuria by 54%. And the benefits? They lasted decades-even after blood sugar control relaxed. That’s called “metabolic memory.” Your body remembers what you did for your kidneys.
For type 2 diabetes, the UKPDS study showed the same pattern: every 1% drop in HbA1c meant a 21% lower risk of kidney damage. That’s not small. That’s life-changing.
But tight control isn’t just about sugar. Blood pressure matters just as much. The KDIGO guidelines say if your UACR is over 300 mg/g, aim for below 120/80 mmHg. But the SPRINT trial showed that pushing systolic pressure below 120 mmHg in some patients increased the risk of sudden kidney injury. So the ADA recommends a more balanced target: under 140/90 for most people with DKD.
The bottom line? You need both. Tight blood sugar and tight blood pressure. And that’s where many patients fall short. NHANES data from 2017-2018 showed only 12.2% of U.S. adults with diabetes hit all three targets: blood sugar, blood pressure, and cholesterol.
Medications That Protect Your Kidneys
Once albuminuria shows up, it’s not enough to just monitor. You need to treat. And the first line is always a drug that blocks the renin-angiotensin-aldosterone system (RAAS)-either an ACE inhibitor or an ARB.
The IRMA-2 trial proved it: giving losartan (100 mg daily) to type 2 diabetes patients with early albuminuria cut their risk of progressing to severe kidney damage by 53%. The rule now? Titrate these drugs to the highest approved dose-even if your blood pressure is already normal. Protection isn’t about lowering pressure. It’s about protecting the filter.
But that’s not all. Since 2023, SGLT2 inhibitors like empagliflozin have become first-line therapy. The EMPA-KIDNEY trial showed they reduced the risk of kidney failure by 28% in patients with UACR above 200 mg/g. And they work even if you’re already on an ACEi or ARB.
Now there’s finerenone, a newer drug that blocks a specific receptor linked to kidney scarring. In trials, it cut albuminuria by 32% in just four months and slowed kidney function decline by 23% over three years. But here’s the catch: only 28.7% of patients with DKD are getting all three recommended therapies-RAAS blocker, SGLT2 inhibitor, and finerenone if needed.
Why So Many People Are Falling Through the Cracks
There’s a massive gap between what we know works and what actually happens in clinics. In one survey, 78% of primary care offices said they don’t have electronic alerts to remind them to order UACR tests. Twenty-three percent of patients don’t return their urine samples. And 41% of providers still don’t fully understand how powerful early albuminuria is as a predictor.
It’s not just about knowledge. It’s about access. Finerenone and SGLT2 inhibitors are expensive. Insurance hurdles delay treatment. Patients skip doses because they feel fine. And in underserved communities, the gap is wider. The CRIC study found that socioeconomic factors explain 63% of why people don’t get the right meds.
But there’s hope. Clinics using point-of-care urine testing cut follow-up loss by 37%. Pharmacist-led teams helped 89% of patients reach maximum drug doses. And clinics with EHR alerts that pop up every year when a UACR is due? They’re seeing better outcomes.

What You Can Do Today
If you have diabetes, here’s your action list:
- Ask for your UACR result every year. Don’t wait for your doctor to bring it up.
- If your result is above 30 mg/g, get two more tests within six months to confirm.
- Work with your doctor to get your HbA1c under 7%-or lower if you’re young and low-risk for low blood sugar.
- Keep your blood pressure under 140/90. If it’s higher, ask if you need a blood pressure pill that also protects your kidneys.
- Ask if you’re on an ACE inhibitor or ARB. If not, why not? If you are, ask if you’re on the highest dose.
- Ask about SGLT2 inhibitors (like empagliflozin or dapagliflozin) or finerenone. These aren’t just for blood sugar-they’re kidney protectors.
Albuminuria isn’t a death sentence. It’s a wake-up call. And the earlier you respond, the more you save-not just your kidneys, but your heart, your energy, your future.
What Happens If You Ignore It?
Left unchecked, diabetic kidney disease doesn’t just fade. It progresses. Albuminuria climbs. Kidney function drops. Eventually, the kidneys fail. At that point, you need dialysis or a transplant. And the damage? It’s permanent.
But here’s the flip side: if you catch albuminuria early and act, you can reverse it. Some patients with moderately increased albuminuria go back to normal levels with tight control. Others stabilize. The goal isn’t always perfection. It’s progress.
The 2024 ADA/KDIGO consensus says that if every diabetic patient got proper screening and treatment, we could prevent 1.2 million new cases of DKD in the U.S. by 2030. That’s 37% fewer people needing dialysis. And $14.8 billion saved in healthcare costs.
That’s not just statistics. That’s real people-parents, grandparents, coworkers-avoiding dialysis chairs, hospital stays, and early death.
It’s not about being perfect. It’s about being consistent. One test. One pill. One blood pressure check. One conversation with your doctor. That’s how you change the trajectory of your health.
What does albuminuria mean for someone with diabetes?
Albuminuria means protein is leaking from your kidneys into your urine, which is the earliest sign of diabetic kidney damage. Even small amounts (above 30 mg/g) indicate injury. It’s not normal and should never be ignored. Catching it early gives you the best chance to stop further damage.
How often should I get tested for albuminuria?
If you have type 2 diabetes, get tested at diagnosis. If you have type 1 diabetes, start testing after five years. Once you’re diagnosed with diabetes, you should get a UACR test every year. If your result is abnormal, you’ll need two more tests within 3 to 6 months to confirm. After that, testing every 3 to 6 months is common if you’re on treatment.
Can albuminuria go away?
Yes, in some cases. With tight blood sugar control, blood pressure management, and medications like ACE inhibitors or SGLT2 inhibitors, some people with moderately increased albuminuria see their levels drop back into the normal range. The key is early, consistent action-not waiting until symptoms appear.
Why do I need to take blood pressure medicine if my pressure is normal?
ACE inhibitors and ARBs aren’t just for lowering blood pressure-they protect your kidney filters directly. Even if your blood pressure is normal, these drugs reduce protein leakage and slow kidney damage. Guidelines recommend using them at the highest tolerated dose for kidney protection, regardless of your BP.
Are new drugs like finerenone and SGLT2 inhibitors really necessary?
Yes. SGLT2 inhibitors reduce kidney failure risk by 28%, and finerenone slows kidney decline by 23% over three years-even when used with ACEi/ARBs. These aren’t optional extras. They’re now standard of care for people with diabetic kidney disease and albuminuria. If your doctor hasn’t mentioned them, ask why.
What if I can’t afford these medications?
Many drug manufacturers offer patient assistance programs. Pharmacies and nonprofit groups can help you apply. Don’t skip treatment because of cost-talk to your doctor or pharmacist. Sometimes, generic ACE inhibitors or ARBs are affordable, and SGLT2 inhibitors may be covered under your plan’s tiered pricing. Your kidneys are worth fighting for.

Ann Romine
January 2, 2026 AT 11:11My grandma had type 2 for 20 years and never got tested for albuminuria until her creatinine was sky-high. By then, it was too late to reverse. I wish someone had told us back then that even a little protein in urine meant something. Now I make sure my whole family gets tested yearly. It’s not glamorous, but it’s the quiet hero of diabetes care.
Sally Denham-Vaughan
January 3, 2026 AT 22:41Just had my UACR done last week - 42 mg/g. Felt like a punch in the gut. But then I read this post and realized it’s not a death sentence. I’m on an ARB now, started walking daily, and cut out soda. Feels weird to be this proactive, but I’d rather be the person who caught it early than the one who didn’t.
Richard Thomas
January 4, 2026 AT 11:54There’s a philosophical weight to albuminuria that rarely gets discussed. It’s not just a biomarker - it’s the body’s silent testimony to years of metabolic compromise. We treat diabetes like a numbers game, but the kidney doesn’t care about HbA1c percentages. It cares about sustained exposure. The fact that we can reverse early damage with consistent care speaks to a deeper truth: biology remembers what we do to it, even when we forget. We’re not just managing disease - we’re negotiating with our own physiology, one urine sample at a time.
Andy Heinlein
January 6, 2026 AT 04:48Just got my SGLT2 script filled! Empagliflozin is a game changer. I thought meds were just for sugar, but now I know they’re for my kidneys too. Feels like I’m finally fighting back instead of just hoping for the best. Also, my energy’s up and I lost 8 lbs without trying. Win win!
Todd Nickel
January 7, 2026 AT 06:14The data on finerenone is compelling, but the real issue is implementation. Most primary care providers are overwhelmed, undertrained, and lack EHR support. A 2023 JAMA study showed that when clinics implemented automated UACR alerts, testing rates jumped from 58% to 89%. The technology exists. The knowledge exists. What’s missing is systemic will. We optimize for efficiency, not outcomes - and kidneys pay the price.
Heather Josey
January 8, 2026 AT 08:11As a nurse practitioner, I see this every day. Patients think if they ‘feel fine,’ they’re fine. But diabetic kidney disease is silent until it’s not. I now have a printed handout I give everyone at diagnosis: ‘Your kidneys don’t complain. You have to ask for their report.’ It’s changed how I practice. And yes - I push for the highest dose of ACEi/ARB, even if BP is normal. Protection isn’t about numbers. It’s about integrity.
Olukayode Oguntulu
January 9, 2026 AT 06:07Typical Western medical reductionism. You reduce a complex systemic metabolic disorder to a single urine biomarker and call it ‘early detection.’ Meanwhile, the real root - industrial food systems, sedentary lifestyles, pharmaceutical profit motives - remains untouched. You prescribe finerenone like it’s a magic bullet, but what about ancestral diets? What about circadian rhythm disruption? The system profits from chronicity. Your ‘early detection’ is just a revenue stream with a stethoscope.
jaspreet sandhu
January 10, 2026 AT 07:40This whole albuminuria thing is overhyped. In India, we’ve seen people with UACR over 1000 and still walking fine. Meanwhile, some with normal levels get dialysis in 2 years. It’s all about genetics and luck. No point stressing over a number. Just eat less sugar, move more, and pray. Medicine in the West is too obsessed with numbers and pills. Real health is simple.
Alex Warden
January 12, 2026 AT 06:27Why are we giving expensive drugs to people who can’t follow basic advice? If you can’t control your sugar, why should taxpayers pay for finerenone? This isn’t healthcare - it’s entitlement. People need to stop blaming doctors and start taking responsibility. No drug fixes laziness. No pill fixes don’t care.
Kristen Russell
January 13, 2026 AT 20:02I got my UACR back at 28. Normal. But I still asked for a repeat test. Better safe than sorry. One test doesn’t define you. Consistency does.
Bryan Anderson
January 14, 2026 AT 20:20Thank you for this thorough breakdown. I’ve been managing type 2 for 14 years and never knew that ACE inhibitors were protective even when BP was normal. My doctor never explained that. I’ve scheduled an appointment to ask about my current meds and whether I’m on the highest tolerated dose. Small changes, big impact.
Liam George
January 14, 2026 AT 21:10Albuminuria is just a tool to sell more drugs. The real agenda? Pharma wants you dependent. They invented ‘microalbuminuria’ to turn millions into patients. SGLT2 inhibitors? They were designed to fail in heart trials first. Now they’re repackaged as kidney saviors. The data is cherry-picked. The side effects - yeast infections, DKA, amputations - are buried in the fine print. Don’t trust the system. Question everything.
sharad vyas
January 15, 2026 AT 12:30In my village in Punjab, we used to say, ‘The body speaks in whispers before it screams.’ We didn’t have UACR tests, but we watched for swelling, tiredness, and changes in urine color. My uncle had diabetes for 30 years. He drank neem water, walked every morning, and never took pills. He lived to 87. Maybe the answer isn’t just in labs, but in tradition and rhythm.
Bill Medley
January 16, 2026 AT 10:52Well-researched and clinically precise. The integration of DCCT, UKPDS, EMPA-KIDNEY, and SPRINT data into a coherent clinical narrative is exemplary. This represents the current standard of evidence-based care.
Paul Ong
January 17, 2026 AT 10:17Just started finerenone last month. My doc said it’s a game changer. I’ve been on an ARB for years. Now I’m on three meds. I feel fine. But I’m not taking it for granted. I check my BP daily. I log my meals. I walk after dinner. This isn’t a cure. It’s a daily practice. One step at a time