Electrolyte Imbalances: How to Manage Potassium, Phosphate, and Magnesium in Kidney Health
 Dec, 27 2025
Dec, 27 2025
When your kidneys aren’t working right, your electrolytes pay the price. Potassium, phosphate, and magnesium don’t just float around in your blood-they’re doing the heavy lifting for your heart, muscles, and nerves. Too little or too much of any one of them can send you to the ER. And if you have kidney disease, diabetes, or are on diuretics, you’re at higher risk. The good news? These imbalances are often preventable-and treatable-if you know what to look for and when to act.
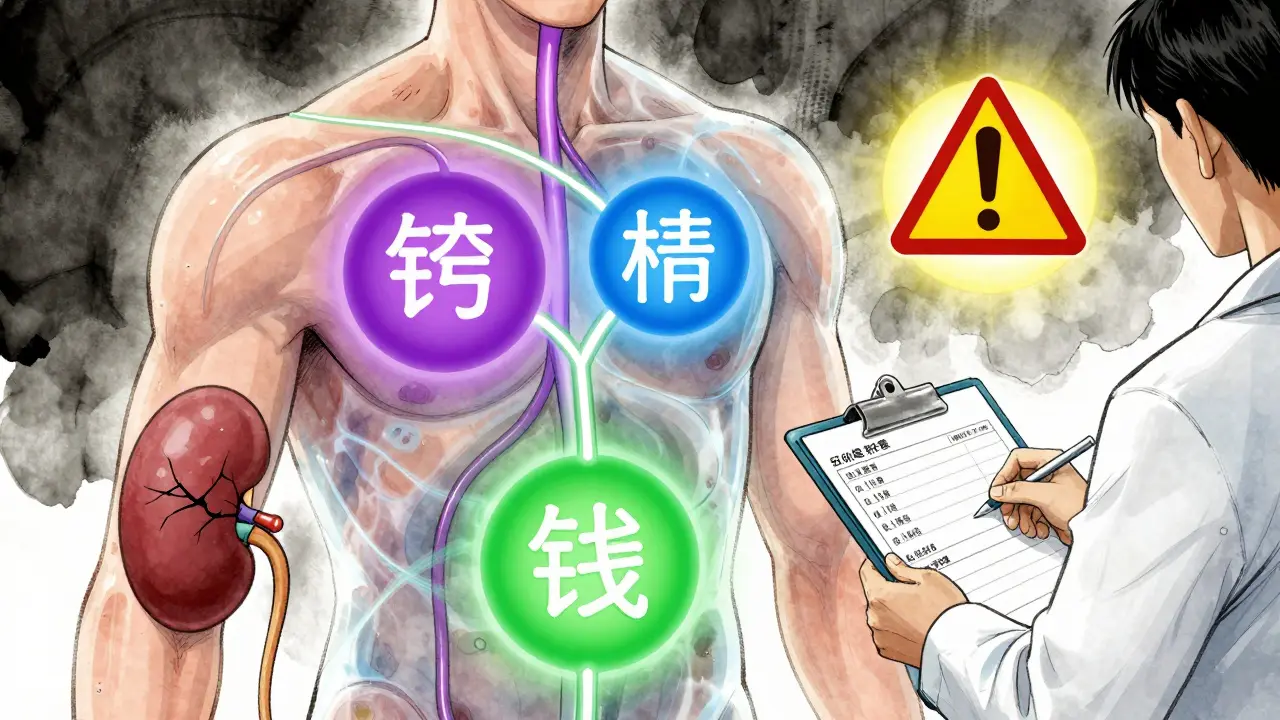
Why These Three Electrolytes Matter
Potassium keeps your heartbeat steady. If it drops below 3.2 mEq/L, you might feel weak, dizzy, or get muscle cramps. If it spikes above 5.0 mEq/L, your heart can start fluttering dangerously. Phosphate is how your cells make energy. When levels fall below 2.5 mg/dL, you can struggle to breathe-even if you’re not sick with pneumonia. Magnesium is the quiet helper behind 300+ enzyme reactions. Low magnesium doesn’t just cause muscle twitches; it makes low potassium impossible to fix, no matter how much you give.
These aren’t isolated numbers. They talk to each other. Low magnesium causes low potassium. Low phosphate can crash after a sugar-heavy IV drip or iron infusion. High potassium? Often tied to kidney failure or meds like ACE inhibitors. And here’s the kicker: treating one without checking the others can make things worse.
Normal Ranges and When to Worry
Here’s what healthy levels look like:
- Potassium: 3.2-5.0 mEq/L
- Magnesium: 1.7-2.2 mg/dL (or 0.7-0.9 mmol/L)
- Phosphate: 2.5-4.5 mg/dL
But numbers alone don’t tell the whole story. Critical danger zones are clear:
- Potassium under 3.0 or over 6.5 mEq/L? Emergency.
- Magnesium under 1.0 or over 2.5 mg/dL? Time to act.
- Phosphate under 1.0 mg/dL? You’re at risk for respiratory failure.
These thresholds aren’t arbitrary. They’re based on real cases where people went into cardiac arrest or stopped breathing because their labs were ignored. In 2022, a study at Vanderbilt University showed that hospitals using strict protocols cut death rates from electrolyte issues by nearly 20%.
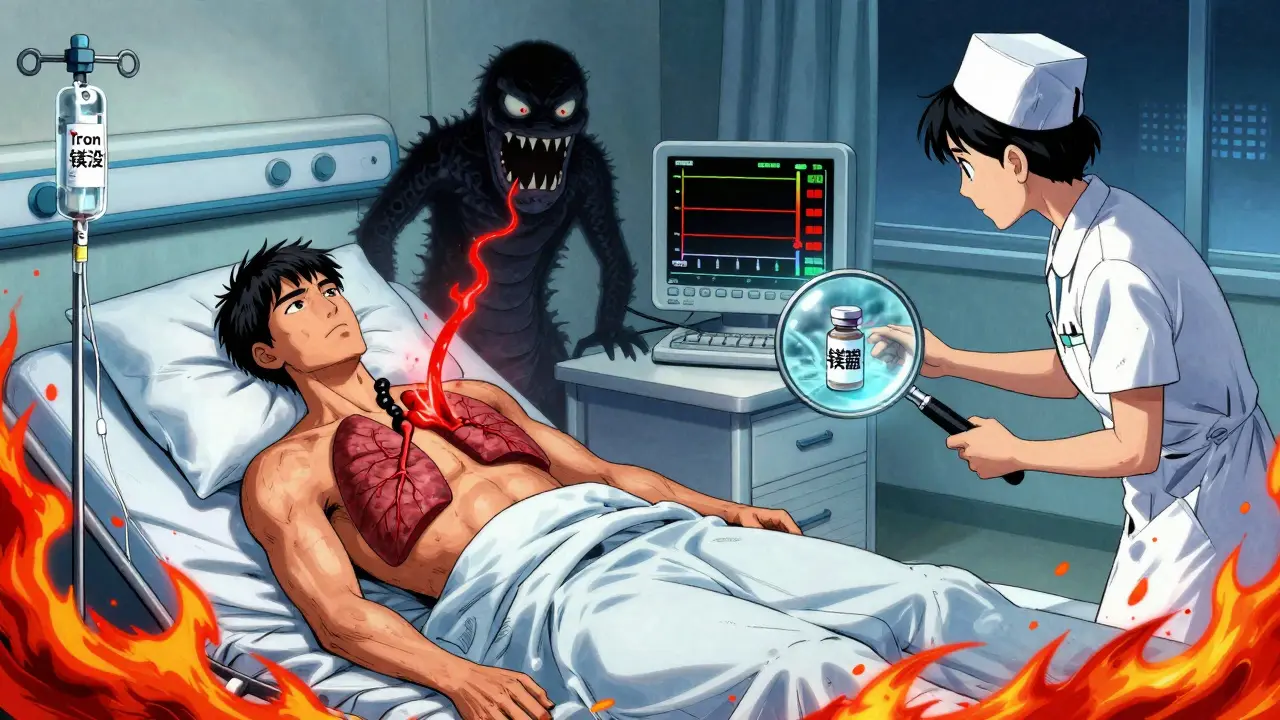
How Low Potassium Happens-and Why Magnesium Is the Key
Low potassium (hypokalemia) is common in people on water pills, with vomiting, or with kidney disease. But here’s what most doctors miss: if magnesium is low, giving potassium won’t help. Your kidneys just keep flushing it out.
That’s why the rule is simple: check magnesium before you give potassium. If magnesium is under 1.8 mg/dL, give 4 grams of magnesium sulfate over 30-60 minutes-usually as a premixed IV bag. Wait an hour. Then check potassium again. Often, it rises on its own.
And don’t just give a single dose. If you’re treating someone with heart failure or on long-term diuretics, you’ll need ongoing magnesium. Oral supplements like magnesium oxide or citrate can help, but IV is faster in acute cases. Studies show that patients with both low potassium and low magnesium have three times the risk of dangerous heart rhythms than those with just low potassium.
Phosphate: The Silent Crisis in Hospitals
Phosphate doesn’t get much attention-until someone can’t breathe. Hypophosphatemia is common in critically ill patients, especially after refeeding, alcohol withdrawal, or severe infections. But one of the biggest hidden causes? Iron infusions.
In 2020, the FDA issued a safety alert: high-dose ferric carboxymaltose (a common iron treatment for anemia) can cause phosphate to crash by up to 50% within days. Many patients get discharged after an iron drip, then end up back in the hospital with fatigue, confusion, and trouble breathing. It’s not rare-it’s predictable.
Management? If phosphate is below 1.5 mg/dL, give IV phosphate-usually 7.5 mmol in 100 mL of fluid over 4-6 hours. Oral phosphate (8 mmol tablets) works for mild cases. But don’t go too fast. Too much phosphate too quickly can cause calcium to drop or lead to calcification in soft tissues. Always check calcium and magnesium at the same time.
High Potassium: The Silent Killer
Hyperkalemia (high potassium) is scary because it can kill before you feel anything. ECG changes-peaked T waves, wide QRS-can appear suddenly. Patients with kidney disease, diabetes, or on blood pressure meds like ACE inhibitors or ARBs are most at risk.
For potassium over 7.0 mEq/L with ECG changes, you need immediate action:
- Give calcium gluconate (10-20 mL IV) to protect the heart-this doesn’t lower potassium, but it stops the heart from going haywire.
- Give insulin (10 units) with 50g of glucose (D50) to push potassium into cells. Effects start in 15 minutes.
- Use a potassium binder like patiromer or sodium zirconium cyclosilicate (approved by NICE in early 2023). These aren’t old-school kayexalate-they’re safer and work in the gut to trap potassium.
- If all else fails, dialysis. Especially if the patient has advanced kidney disease.
After treatment, check potassium at 1, 2, 4, 6, and 24 hours. It can rebound. And if you’re on a potassium binder, don’t forget to check magnesium and phosphate too-these meds can pull them down as well.
Monitoring: When and How Often
Checking electrolytes once isn’t enough. Timing matters.
- After treating hyperkalemia: check potassium at 1, 2, 4, 6, and 24 hours.
- After giving magnesium: check again in 6-12 hours to see if levels held.
- After phosphate replacement: check calcium every 4-6 hours for 24 hours to catch drops.
- For anyone on diuretics, ACE inhibitors, or iron infusions: check electrolytes every 3-5 days if they’re outpatients.
Emergency departments now use point-of-care testing-results in under 10 minutes. That’s cut the time to treatment by over 30 minutes on average. If you’re in a hospital, ask: “Can we get a stat electrolyte panel?”
What to Avoid
Here are common mistakes that make things worse:
- Giving potassium without checking magnesium first.
- Using oral potassium too fast-it can burn your stomach and cause ulcers.
- Ignoring phosphate in patients getting IV glucose or insulin.
- Using calcium gluconate for low calcium without checking magnesium-low magnesium makes calcium stubborn.
- Assuming a normal potassium level means everything’s fine. Look at trends. A drop from 4.8 to 3.9 in 48 hours? That’s a red flag.
Long-Term Management for Kidney Patients
If you have chronic kidney disease, you’re more likely to have recurring imbalances. Work with your nephrologist on a plan:
- Limit high-potassium foods (bananas, potatoes, spinach, tomatoes) if your levels are high.
- Take phosphate binders with meals if your phosphate is high-but avoid overuse, which can cause low phosphate.
- Consider magnesium supplements if you’re on loop diuretics (like furosemide) and get muscle cramps.
- Ask about newer potassium binders if you’re on multiple meds that raise potassium.
Recent trials are testing personalized treatment based on genetics-some people naturally lose more potassium or magnesium in urine. These “genotype-guided” protocols are in phase 3 trials and could change how we treat kidney patients by 2026.
Bottom Line: Think in Systems, Not Single Numbers
Electrolytes don’t work alone. You can’t fix potassium without checking magnesium. You can’t treat phosphate without watching calcium. And you can’t manage any of them without knowing the patient’s meds, kidney function, and diet.
The goal isn’t just to get numbers into range-it’s to stop the chain reaction before it starts. Hospitals that use checklists and alerts for electrolytes have seen 22% fewer bad outcomes since 2021. You don’t need to be a doctor to ask: “Did you check magnesium before giving potassium?” or “Is phosphate on the panel?”
If you or someone you care for has kidney disease, diabetes, or is on diuretics or iron infusions, make electrolyte checks part of every doctor visit. Keep a log. Track trends. Speak up. These imbalances are silent-but they don’t have to be deadly.
Can low magnesium cause low potassium even if I’m not on diuretics?
Yes. Magnesium helps your kidneys hold onto potassium. If magnesium is low, your body will keep flushing potassium out-even if you’re not taking water pills. This is why doctors now check magnesium before treating low potassium. Without fixing magnesium first, potassium levels often won’t improve no matter how much you give.
Is it safe to take magnesium supplements if I have kidney disease?
It depends. Healthy kidneys can handle extra magnesium, but if your kidney function is below 30%, you’re at risk for magnesium buildup. Symptoms include drowsiness, low blood pressure, or muscle weakness. Always talk to your nephrologist before starting supplements. Blood tests are key-don’t guess.
Can iron infusions really cause phosphate to drop?
Yes. High-dose ferric carboxymaltose, a common iron infusion for anemia, has been linked to sudden drops in phosphate since the FDA issued a safety alert in 2020. Patients often feel fine after the infusion, then get extremely tired or short of breath days later. Always ask for a phosphate check 3-5 days after an iron drip, especially if you have kidney disease.
What’s the fastest way to raise potassium if I’m having symptoms?
For mild low potassium (3.0-3.2 mEq/L), oral potassium citrate or chloride tablets work well. For severe symptoms like muscle weakness or palpitations with levels under 3.0, IV potassium is needed-but only in a hospital. Never give yourself IV potassium at home. It’s dangerous. Speed matters: IV potassium should never be given faster than 10 mEq per hour through a peripheral line.
Why do I need to check calcium when treating low phosphate?
When you give phosphate, it binds to calcium in your blood. This can cause calcium levels to drop suddenly, leading to tingling, muscle spasms, or even seizures. That’s why doctors check calcium every 4-6 hours after phosphate replacement. If calcium drops too low, they’ll give calcium gluconate. It’s a balancing act.
Electrolyte imbalances aren’t just lab results-they’re warning signs your body is under stress. For people with kidney issues, staying ahead of these numbers isn’t optional. It’s life-saving. Know the ranges. Ask the right questions. And never treat one electrolyte without checking the others.

Elizabeth Ganak
December 27, 2025 AT 20:58Just had my potassium drop to 3.1 last month after a bad bout of diarrhea. My doc didn't check magnesium until I insisted. Turned out it was at 1.4. Gave me IV mag and my potassium bounced back in 24 hours. Never skipping that step again.
Also, don't even get me started on how many nurses still think oral potassium is safe to chug like juice. Please.
Thank you for this post. Real talk needed.
Nicola George
December 29, 2025 AT 04:05Oh so now we’re doing electrolyte bingo? Low mag, low pot, low phos - just add a dash of iron infusion and you’ve got yourself a full house.
Meanwhile my nephrologist still thinks ‘just eat more bananas’ is a treatment plan.
Raushan Richardson
December 30, 2025 AT 08:04This is the kind of info that saves lives. Seriously. I’m a nurse and I’ve seen so many patients get sent home with ‘normal’ labs but their magnesium was quietly tanking.
Don’t just look at the numbers - look at the story behind them. If someone’s cramping, fatigued, or has weird heart flutters? Check mag before you even think about K.
And if you’re on diuretics? You’re basically on a slow drip of electrolyte loss. Get checked every 3 weeks, no excuses.
dean du plessis
December 30, 2025 AT 15:16Iron infusions causing phosphate crashes is wild. I had one last year and felt fine until three days later when I could barely walk up the stairs. They thought it was depression. Turned out my phosphate was 1.2. Took a week to recover. Why isn’t this common knowledge?
Also magnesium before potassium - yeah that’s basic now but still skipped too often.
Todd Scott
December 30, 2025 AT 17:14It’s fascinating how the body’s electrolyte system operates as a dynamic, interdependent network rather than a series of isolated variables. The kidneys, as the primary regulators of homeostasis, are exquisitely sensitive to pharmacologic interventions - particularly diuretics, ACE inhibitors, and intravenous iron formulations - which can precipitate cascading derangements in potassium, magnesium, and phosphate concentrations. The clinical implications are profound: failure to recognize the bidirectional relationships between these ions often leads to therapeutic inertia, where correction of one parameter exacerbates another. For instance, hypomagnesemia impairs renal tubular reabsorption of potassium, rendering potassium replacement ineffective unless magnesium is simultaneously restored. Similarly, rapid phosphate repletion can induce hypocalcemia due to precipitation of calcium phosphate complexes in soft tissues, a phenomenon that has been documented in post-refeeding syndrome and post-iron infusion scenarios. Recent studies, including those from Vanderbilt and the NICE guidelines, underscore the importance of protocol-driven, multi-parameter monitoring. The future lies in predictive algorithms that integrate genetic polymorphisms in renal transporters - such as TRPM6 and NCC - to personalize electrolyte management. We are moving from reactive correction to proactive, systems-based prevention.
Paula Alencar
January 1, 2026 AT 01:25While I appreciate the clinical precision of this exposition, I must emphasize that the ethical imperative to prioritize patient safety through rigorous, evidence-based electrolyte monitoring cannot be overstated. The failure to implement standardized protocols - particularly the mandatory assessment of magnesium prior to potassium repletion - constitutes a systemic deficiency in contemporary medical practice. In my capacity as a clinical educator, I have observed multiple instances where such oversights led to preventable arrhythmias, respiratory compromise, and even mortality. It is not merely a matter of laboratory values; it is a matter of professional accountability. Hospitals that have adopted mandatory electrolyte checklists, as referenced in the 2021 outcomes study, have demonstrated not only improved survival metrics but also enhanced interdisciplinary communication. The time for ad hoc, reactive medicine is over. We must institutionalize vigilance.
Nikki Thames
January 2, 2026 AT 10:37Of course they’re telling you to check magnesium before potassium - because the pharmaceutical industry doesn’t want you to know that real healing comes from fasting, alkaline diets, and sunlight.
IV magnesium? Please. That’s just another way to keep you dependent on the system.
And iron infusions causing phosphate crashes? That’s not science - that’s a cover-up. The FDA is in bed with Big Pharma. Your kidneys don’t need ‘fixing’ - they need detoxing. Eat more sea salt. Drink lemon water. Stop trusting labs.
And if your doctor doesn’t mention ‘cellular resonance’ or ‘biofield harmonics,’ they’re not your real healer.
Chris Garcia
January 4, 2026 AT 05:19In the African tradition, we say: the river does not flow in one direction - it whispers through stones, bends around roots, and carries the memory of rain. So too with electrolytes. Potassium is the drumbeat, magnesium the hidden rhythm beneath, phosphate the breath of the cell. To treat one without listening to the others is to dance to only half the song.
When I was young, my grandmother would say: ‘If your hand trembles, check the soil - not just the seed.’ The body is soil. The lab is the weather. And we, the healers, must learn to read both.
Western medicine has mapped the body like a machine. But the body is a song. And songs are not fixed - they are felt.
James Bowers
January 5, 2026 AT 08:31The assertion that magnesium deficiency impedes potassium correction is not universally supported by high-quality randomized controlled trials. While observational data suggest an association, confounding variables - including concurrent diuretic use, gastrointestinal losses, and dietary intake - are inadequately controlled in the cited literature. Furthermore, the recommendation to administer 4 grams of IV magnesium sulfate as a routine protocol lacks robust phase III validation. The FDA’s safety alert regarding ferric carboxymaltose is based on case reports, not prospective cohort studies. Until longitudinal data confirms causality and clinical benefit, such protocols risk over-treatment and iatrogenic harm. This post, while well-intentioned, promotes a reductionist approach that may lead to unnecessary interventions and increased healthcare costs.
Olivia Goolsby
January 6, 2026 AT 20:32Wait - so you’re telling me that the entire medical establishment is lying about electrolytes? That magnesium isn’t just ‘a supplement’ but the real key? That iron infusions are secretly destroying people’s phosphate levels? And that they’ve been hiding this since 2020? And now they’re pushing ‘potassium binders’ like they’re magic pills? And dialysis is the only real solution - but they don’t want you to know that because they make billions off the system?
What about the 2023 NICE guidelines? They’re just a front for Big Pharma’s new profit stream - patiromer and zirconium cyclosilicate? They’re not ‘safer’ - they’re just more expensive. And why does everyone keep saying ‘check magnesium’? Because the labs don’t bill for it unless you code it as ‘unspecified hypomagnesemia’ - that’s the real reason!
And what about the fact that all these ‘normal ranges’ were set by a committee that includes people who own stock in renal drug companies? I’ve seen the documents. They’re not ‘normal’ - they’re manufactured.
Don’t trust the labs. Don’t trust the doctors. Don’t trust the ‘protocols.’
Go to the mountains. Fast. Drink spring water. And if your potassium drops? Don’t call 911 - call your spirit guide.