Frequent Urination and Urgency from Medications: Common Bladder Side Effects
 Dec, 15 2025
Dec, 15 2025
Medication Side Effect Calculator
Check Your Risk
Enter your medication details and symptoms to see if they might be causing your bladder issues.
Your Results
Waking up three times a night to pee? Feeling a sudden, sharp urge to go even when your bladder doesn’t feel full? You’re not alone-and it might not be aging or drinking too much coffee. More than one in five adults taking common medications report these exact symptoms, and many never connect them to what’s in their pillbox. Frequent urination and urinary urgency are among the most overlooked side effects of prescription drugs, especially in people over 40 who take multiple medications. The problem is real, widespread, and often fixable-if you know what to look for.
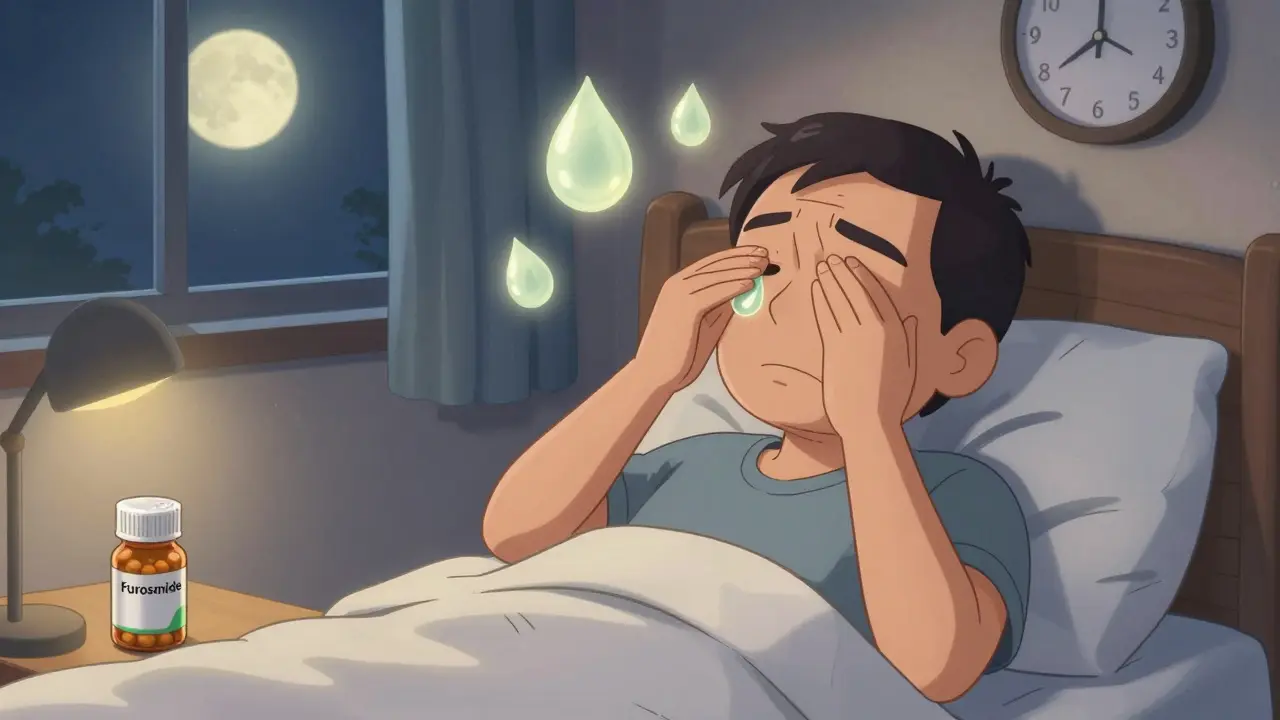
Diuretics Are the Top Culprit
Diuretics, often called water pills, are the most common cause of frequent urination from medications. Drugs like hydrochlorothiazide, furosemide (Lasix), and spironolactone (Aldactone) are prescribed for high blood pressure, heart failure, and swelling. But they work by forcing your kidneys to dump more fluid into your urine. That means more trips to the bathroom-sometimes up to 12 times a day.
Studies show that about 65% of people taking diuretics experience increased daytime urination, and 40% wake up at night to pee. The higher the dose, the worse it gets. One 2021 study found that patients on 80mg of furosemide daily were nearly four times more likely to need incontinence products than those on 20-40mg. The good news? Timing matters. Taking your diuretic before 2 p.m. can cut nighttime bathroom trips by 60%, according to clinical data from BuzzRx. That simple change alone helps thousands avoid sleep disruption and falls.
Calcium Channel Blockers and Nighttime Voiding
If you’re on a blood pressure medication like amlodipine, nifedipine, or verapamil, you might be surprised to learn it could be making you pee more at night. These drugs relax blood vessels to lower pressure-but they also interfere with the bladder’s ability to contract properly. The result? Your bladder fills up but doesn’t signal strongly enough to empty completely. That leads to frequent urges, especially after midnight.
Research from the Journal of Hypertension shows that people taking nifedipine average 1.8 more nighttime bathroom visits than those not on the drug. Verapamil carries the highest risk, with 42% of users reporting severe nocturia. Symptoms usually show up within 2-4 weeks of starting the medication. Many patients assume it’s just getting older-but if you started a new blood pressure pill and suddenly can’t sleep through the night, it’s worth a conversation with your doctor.
Antidepressants and Mood Stabilizers: Hidden Bladder Triggers
Antidepressants like venlafaxine (Effexor), escitalopram (Lexapro), and fluoxetine (Prozac) are linked to worsening overactive bladder symptoms in about 22% of users. These drugs affect serotonin and norepinephrine, which play roles in bladder control. Even if your mood improves, you might start feeling like your bladder is in overdrive.
Lithium, used for bipolar disorder, has a unique and serious effect. About 1% of long-term users develop nephrogenic diabetes insipidus-a condition where the kidneys can’t concentrate urine. That means producing 3 liters or more of urine a day. In one study of 873 patients, 9% stopped lithium because of urinary problems. If you’re on lithium and suddenly need to pee every hour, don’t ignore it. Blood tests and kidney function checks can confirm the issue, and your doctor may adjust your dose or add desmopressin to help.
Antipsychotics like clozapine, risperidone, and olanzapine can also cause trouble. They block acetylcholine, a chemical that helps the bladder contract. That leads to incomplete emptying, which feels like urgency and frequent trips-but for a different reason than diuretics. The bladder fills slowly, then suddenly overflows. It’s not always obvious, and many patients think they have a weak bladder when it’s actually a medication effect.
Other Surprising Medications That Affect Your Bladder
Even common over-the-counter drugs can cause problems. Antihistamines like diphenhydramine (Benadryl) and chlorpheniramine (Chlor-Trimeton) relax the detrusor muscle in your bladder. That sounds helpful-but it can lead to urinary retention. When the bladder can’t empty fully, it overfills and leaks. That’s called overflow incontinence, and it’s often mistaken for an overactive bladder.
ACE inhibitors like captopril and ARBs like losartan can cause a persistent cough. That cough puts pressure on the pelvic floor and leads to stress incontinence-leaking when you sneeze, laugh, or lift something. Cleveland Clinic data shows captopril causes this in 15% of users.
Alpha-blockers like tamsulosin (Flomax) and silodosin (Rapaflo) are prescribed for enlarged prostates. They help men urinate better-but they cause retrograde ejaculation in 25-30% of cases. That means semen goes backward into the bladder instead of out through the penis. It’s not dangerous, but it can be shocking if you’re not warned.
What to Do If Medications Are Causing Your Symptoms
The first step? Don’t stop taking your meds on your own. But do track your symptoms. Write down: when you started the medication, when the urinary symptoms began, how often you go, and whether you leak or just feel urgency. Bring this to your doctor.
Most providers now follow a 4-step approach recommended by the Mayo Clinic:
- Check if symptoms started within 2-8 weeks of beginning the medication.
- Rule out infections, prostate issues, or neurological causes with a simple urine test and post-void residual scan.
- Try non-drug fixes: take diuretics before 2 p.m., practice timed voiding (going every 2-3 hours, even if you don’t feel the urge), and do pelvic floor exercises.
- If symptoms persist after 4 weeks, consider switching to a different medication with fewer bladder side effects.
Bladder retraining works. One study showed a 70% success rate after 6-8 weeks of consistent timed voiding and pelvic floor strengthening. Combine that with adjusting when you take your meds, and many people cut their bathroom visits in half.

Why This Is Often Missed
Patients report frustration: 42% of Reddit users in a March 2023 thread said they had to push their doctors to consider medication side effects before any changes were made. Doctors are busy. Urinary symptoms are common in older adults. It’s easy to assume it’s just aging-until someone points out that the problem started the week they added a new pill.
That’s why the International Continence Society now recommends a full medication review for anyone with new-onset urinary symptoms. Especially if they’re on three or more prescriptions. A pharmacist can help flag high-risk drugs too. Don’t wait for your doctor to ask-ask yourself: “Could this be the new pill?”
When to Seek Help
See a urologist or your primary care provider if:
- You’re waking up more than twice a night to pee
- You’re leaking urine without feeling the urge
- You feel like you can’t fully empty your bladder
- Your symptoms started after a new medication
- You’re using incontinence pads daily
There’s no shame in this. Millions of people deal with it. And the good news? In most cases, you don’t have to live with it. Adjusting your meds, timing your doses, or adding simple behavioral strategies can make a huge difference.
What’s Next for Research
Scientists are now looking at genetics to predict who’s more likely to have bladder side effects. Early data suggests people with a specific variant in the CHRM3 gene are 3.2 times more likely to react badly to anticholinergic drugs. This could one day lead to genetic testing before prescribing certain medications-especially for older adults on multiple drugs.
Until then, awareness is your best tool. If you’re taking any of these medications and your bladder feels out of control, talk to your doctor. You might not need to stop the drug-just change how or when you take it. And that small tweak could mean the difference between sleepless nights and a normal life.
Can over-the-counter allergy meds cause frequent urination?
Yes. Antihistamines like diphenhydramine (Benadryl) and chlorpheniramine can relax the bladder muscle, leading to urinary retention. This can cause overflow incontinence, where the bladder overfills and leaks. It’s not frequent urination from overproduction-it’s leakage from incomplete emptying. If you notice new wetting episodes after starting an allergy med, consider switching to a non-sedating alternative like loratadine or cetirizine.
Do all diuretics cause the same level of urinary frequency?
No. Loop diuretics like furosemide are the strongest-they can increase urine output by 50% or more. Thiazides like hydrochlorothiazide are milder, and potassium-sparing diuretics like spironolactone have the least effect on urine volume. But even mild diuretics can cause problems if taken late in the day. The key isn’t just the drug class-it’s timing and dose.
Can I just stop taking my medication if it’s causing bladder issues?
Never stop a prescribed medication without talking to your doctor. Stopping blood pressure or psychiatric meds suddenly can be dangerous. Instead, work with your provider to adjust the dose, change the timing, or switch to a different drug with fewer bladder side effects. Most issues can be managed without quitting the treatment you need.
How long does it take for bladder symptoms to improve after changing a medication?
It varies. If you switch a diuretic to an earlier time, you might notice fewer nighttime trips within 2-3 days. For drugs like calcium channel blockers or antidepressants, it can take 1-4 weeks for symptoms to ease after stopping or reducing the dose. Behavioral changes like timed voiding and pelvic floor exercises usually show improvement after 6-8 weeks of consistent practice.
Are there any natural remedies that help with medication-induced urinary urgency?
There’s no proven natural cure, but behavioral strategies work well. Bladder retraining, pelvic floor exercises (Kegels), and avoiding bladder irritants like caffeine, alcohol, and artificial sweeteners can reduce urgency. Drinking enough water (but not too much before bed) helps too. Some people find acupuncture or biofeedback helpful, but these should support-not replace-medical advice.

Cassandra Collins
December 15, 2025 AT 14:54Mike Smith
December 16, 2025 AT 18:37Ron Williams
December 17, 2025 AT 04:48Kitty Price
December 18, 2025 AT 09:38Billy Poling
December 18, 2025 AT 15:51Souhardya Paul
December 19, 2025 AT 19:04Josias Ariel Mahlangu
December 19, 2025 AT 23:49Arun ana
December 21, 2025 AT 03:23Kayleigh Campbell
December 21, 2025 AT 23:12Andrew Sychev
December 22, 2025 AT 22:34