Fungal Infections Explained: Candida, Athlete’s Foot, and How Antifungal Treatments Really Work
 Nov, 10 2025
Nov, 10 2025
Most people think fungal infections are just a nuisance-itchy feet, a little flakiness, maybe some redness. But if you’ve had one, you know it’s more than that. It lingers. It comes back. And no matter how much you scrub, it won’t just disappear on its own. Athlete’s foot and candida infections aren’t rare. They’re common, stubborn, and often misunderstood. In fact, about 15% of the world’s population has a fungal skin infection at any given time. For women, the odds of getting a yeast infection in their lifetime? 75%. That’s not an outlier. That’s the norm.
What’s Really Causing Your Itch?
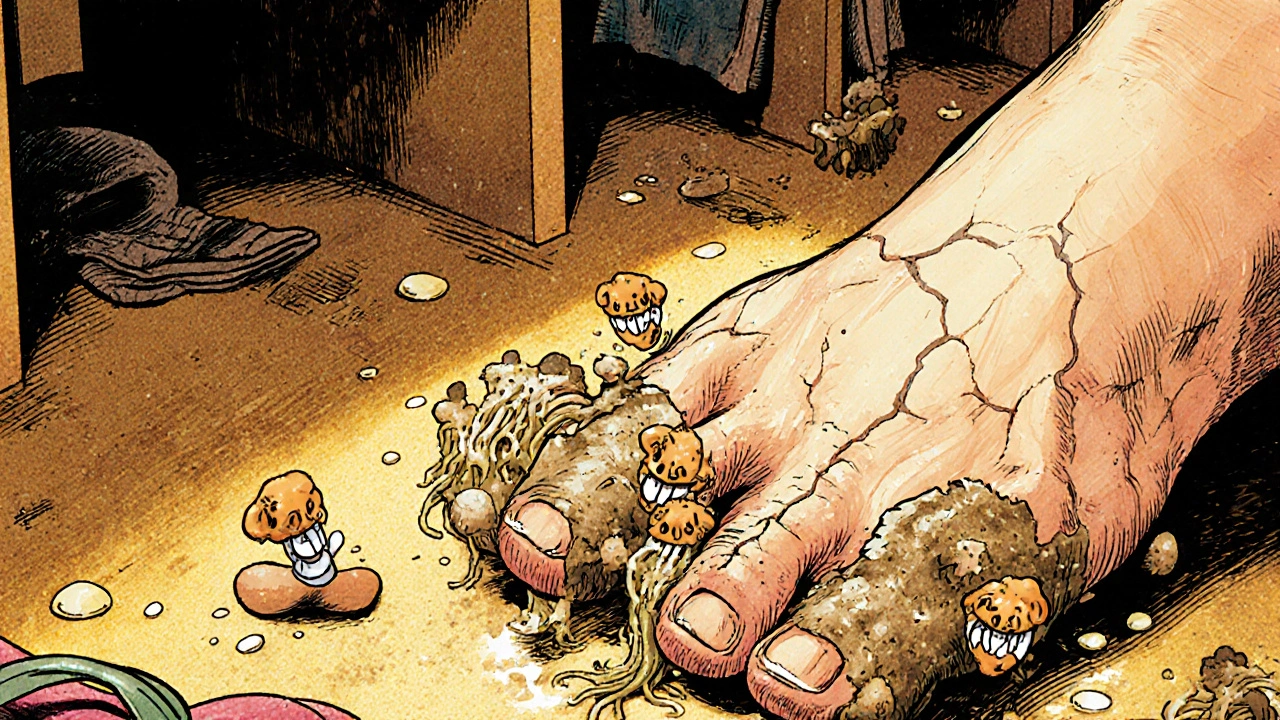
Not all fungal infections are the same. The two biggest players are dermatophytes and Candida. They look similar on the surface-red, flaky, itchy-but they behave completely differently.Athlete’s foot, or tinea pedis, is caused by dermatophytes. These fungi don’t just live on your skin-they eat it. Specifically, they feed on keratin, the tough protein in your skin, nails, and hair. That’s why they love your feet. Warm, sweaty, enclosed in shoes all day? Perfect. They thrive in locker rooms, public showers, and damp towels. The most common types are Trichophyton rubrum and Epidermophyton floccosum. You don’t need to be an athlete to get it. Just walk barefoot in a gym, share shoes, or wear the same socks for days.
Candida, on the other hand, is a yeast. The most common species is Candida albicans. It’s already living in your mouth, gut, and vagina-usually harmless. But when your immune system is off, your skin stays wet, or you’ve taken antibiotics, it overgrows. That’s when you get thrush, vaginal yeast infections, or skin rashes in warm folds like under the breasts or in the groin. Unlike dermatophytes, Candida doesn’t need keratin. It can invade moist, non-keratinized areas too. That’s why it can turn into something serious in people with diabetes or weakened immune systems.
How Do You Know Which One You Have?
Athlete’s foot doesn’t show up the same way every time. There are three main types:- Interdigital-the most common. Affects 70% of cases. Peeling, cracking skin between the toes, especially between the fourth and fifth. Often smells bad.
- Moccasin type-20% of cases. Dry, scaly skin on the soles and sides of the feet. Looks like chronic dryness, so people ignore it… until it spreads.
- Vesicular/bullous-10% of cases. Small blisters that pop and leave raw patches. Can be mistaken for a bacterial infection.
Candida infections look different depending on where they are:
- Oral thrush-white patches on the tongue or inside the cheeks that bleed if scraped.
- Vaginal yeast infection-thick, white discharge, intense itching, burning during urination.
- Cutaneous candidiasis-bright red rash with small pustules around the edges, often in skin folds.
Here’s the catch: if your athlete’s foot looks swollen, oozing, or you have a fever, it’s probably not just fungus anymore. That’s a bacterial infection on top of it-cellulitis. Same goes for candida in someone with diabetes or HIV. What starts as a mild rash can turn life-threatening fast.
What Actually Works? Antifungal Treatments Compared
You’ve probably tried clotrimazole cream. Maybe it helped for a few days. Then it came back. That’s because most people stop too soon. Fungal infections don’t vanish when the itching stops. The fungus is still there, hiding.Topical treatments are the first line. Here’s what’s out there:
- Clotrimazole and miconazole-azoles. Kill fungi by breaking down their cell membranes. Works for mild cases. Cure rate: 70-80% if used correctly.
- Terbinafine (Lamisil)-allylamine. Kills fungi faster. More effective than azoles. One study showed 6-month recurrence rates dropped from 40% with clotrimazole to just 18% with terbinafine.
- Whitfield’s ointment-a mix of salicylic acid and benzoic acid. Doesn’t kill the fungus directly. Instead, it peels away dead skin so the antifungal can reach deeper. Works especially well for interdigital athlete’s foot. One trial found 65% clearance at 4 weeks, compared to 55% with clotrimazole alone.
But here’s the problem: topical treatments only go so deep. If the infection’s in your nails or has spread to your ankles, you need oral meds.
- Terbinafine (250 mg daily for 2-6 weeks)-first choice for stubborn cases. 85% cure rate for athlete’s foot.
- Itraconazole (200 mg daily for 1-2 weeks)-good for people who can’t take terbinafine. Works on both dermatophytes and some Candida.
- Fluconazole (150 mg weekly for 2-4 weeks)-the go-to for vaginal yeast infections and oral thrush.
And yes, there’s new stuff. In 2021, the FDA approved Ibrexafungerp for yeast infections-the first new antifungal class in 20 years. And in early 2023, a new topical drug called olorofim showed 82% success in treating resistant athlete’s foot in clinical trials. It’s not on shelves yet, but it’s coming.

Why Do These Infections Keep Coming Back?
If you’ve had this before, you know the frustration. You treat it. It’s gone. Then, two months later-same spot. Why?Recurrence rates are high. Up to 40% of people who use only topical treatments get it back within a year. Why? Three reasons:
- You stopped too early. Symptoms fade in 3-5 days. But the fungus is still alive. You need to keep applying the cream for at least 1-2 weeks after everything looks normal.
- You didn’t clean your environment. Fungi live in your shoes, socks, shower floor, and towels. If you treat your foot but keep wearing the same dirty socks, you’re re-infecting yourself.
- You have an underlying issue. Diabetes, poor circulation, or a weakened immune system makes it harder to fully clear the infection. That’s why people with diabetes are told to check their feet daily.
One Reddit user, ‘FootFungusFighter’, said: “Clotrimazole failed for 3 weeks. Terbinafine cream cleared it in 10 days.” That’s not magic. It’s science. Terbinafine kills faster and penetrates deeper. But even then, he had to keep his feet dry and change his shoes.
How to Actually Prevent It
Prevention isn’t about being clean. It’s about being dry.- Dry between your toes after every shower. Use a hairdryer on low if needed. Moisture is the #1 trigger.
- Change socks daily. Cotton or moisture-wicking blends only. No synthetic fibers.
- Don’t walk barefoot in gyms, pools, or locker rooms. Wear flip-flops.
- Rotate your shoes. Let them air out for 24-48 hours between wears. Fungi live in leather and foam.
- Use antifungal powder in shoes and socks. Powder with 2% miconazole works better than plain talc.
- Don’t share towels. Fungi spread through skin flakes. A single towel used by two people can carry infection for weeks.
And here’s a tip most people miss: if you have athlete’s foot, treat your nails too. Fungi can hide under the nail and re-infect your skin. Same goes for jock itch-if you have it, don’t put cream on your groin and then wipe your feet with the same towel.

When to See a Doctor
You don’t need to run to the clinic for a mild case. But if any of these happen, it’s time:- Your skin is swollen, hot, or oozing pus.
- You have a fever.
- You have diabetes and even a small crack on your foot.
- It’s been 4 weeks of treatment and it’s not improving.
- You keep getting it back, even with proper hygiene.
Doctors can do a skin scraping test. It’s quick. No needles. Just a little scrape, put under a microscope, and they’ll know if it’s fungus, bacteria, or something else. No more guessing.
And here’s the hard truth: fungal infections are getting harder to treat. A new strain of athlete’s foot fungus, Trichophyton indotineae, is resistant to common antifungals. First seen in India in 2017, it’s now in 28 countries. The WHO lists it as a priority pathogen. That’s why using the right treatment, and finishing it, matters more than ever.
What’s Next?
The good news? Most fungal infections are easy to fix-if you treat them right. The CDC’s ‘My Action Plan’ for diabetes patients cut recurrent infections by 35% just by teaching people how to check their feet and keep them dry. That’s not a miracle drug. That’s education.Antifungal resistance is rising. New drugs are coming. But until then, the best treatment is still: know what you’re dealing with, use the right medicine, finish the course, and keep your skin dry. It’s simple. It’s boring. But it works.

Andrew Forthmuller
November 12, 2025 AT 12:54Terbinafine worked for me in 5 days. Clotrimazole? Waste of time.
Benjamin Stöffler
November 13, 2025 AT 00:40Let’s be honest-fungi aren’t ‘infections’; they’re evolutionary reminders that we’re just warm, moist meat sacks trying to outwit microbial anarchists. Dermatophytes? They’re not invaders-they’re tenants who never got evicted. And Candida? It’s not ‘overgrowing’-it’s just waiting for your immune system to take a nap. You treat symptoms, but the real problem is the ecosystem you’ve cultivated: sugar, stress, and synthetic socks. The fungus doesn’t hate you-it’s just better at surviving than you are.
Antifungals? They’re Band-Aids on a leaking dam. Until we stop treating the body like a battlefield and start treating it like a garden, we’ll keep re-seeding the same weeds. And yes, I’ve read the WHO report. Trichophyton indotineae isn’t a ‘new strain’-it’s the logical endpoint of a global culture that treats hygiene like an option.
We need systemic change: public shower regulations, antifungal prophylaxis for diabetics, and a cultural shift away from ‘scrub harder’ nonsense. Dryness isn’t a tip-it’s a bioethical imperative.
Samantha Wade
November 13, 2025 AT 11:24Thank you for this comprehensive and scientifically accurate overview. It is refreshing to encounter content that not only educates but also emphasizes evidence-based practices over anecdotal remedies. The distinction between dermatophytes and Candida is crucial, and the data on recurrence rates underscores the importance of adherence to treatment protocols. I particularly appreciate the inclusion of emerging treatments such as ibrexafungerp and olorofim, as these represent meaningful progress in a field long neglected by pharmaceutical innovation. Continued public education on fungal hygiene is essential to reducing transmission and preventing complications, especially among vulnerable populations.
Elizabeth Buján
November 13, 2025 AT 21:16okay but like… i had a yeast infection after antibiotics and i thought i was dying. then i used fluconazole and it was like magic. but then i did it again 3 months later and i was like… why am i like this??
turns out i was wearing gym socks for 3 days straight and my underwear was cotton but my pants were synthetic and i was just… sweating in a bubble. now i dry my toes with a hairdryer like it’s a sacred ritual. also i rotate shoes like they’re exes. it’s weird but it works. you’re not broken-you’re just living in a fungus paradise and nobody told you.
manish kumar
November 15, 2025 AT 07:34This is one of the most thorough and well-structured explanations I’ve ever read on fungal infections. As someone from India, where athlete’s foot is practically a rite of passage due to shared bathroom facilities and humid climates, I can confirm every point. The rise of Trichophyton indotineae is no myth-it’s a daily reality in urban clinics. I’ve seen patients treated with terbinafine for six weeks, only to relapse because they didn’t decontaminate their footwear. Many don’t even know that their sandals harbor fungal spores for months. We need public health campaigns, not just blog posts. Schools should teach foot hygiene like handwashing. And pharmacies should offer free antifungal powder with every prescription. The science is here; the infrastructure is not. Let’s not wait for another pandemic to realize that fungi don’t care about borders.
Nicole M
November 16, 2025 AT 10:07so i used whitfield’s ointment last year and it was a game changer. nobody talks about it. it’s like the secret weapon. i was using clotrimazole for weeks and nothing. then my cousin said ‘try the acid stuff’ and boom-gone in two weeks. why isn’t this in every drugstore?
Arpita Shukla
November 17, 2025 AT 05:34Interesting that you mention olorofim. The phase 2 trial data from 2023 showed 82% efficacy, but the sample size was only 120 patients. Also, it’s only active against Ascomycota, so it won’t touch Candida glabrata. You’re oversimplifying the resistance landscape. And terbinafine resistance? Still rare. The real threat is azole-resistant Candida auris. That’s the silent epidemic. Not athlete’s foot.
Mark Rutkowski
November 17, 2025 AT 23:49There’s something deeply poetic about fungi. They don’t rage. They don’t scream. They just… wait. They wait for your sweat. They wait for your stress. They wait for your forgotten socks. And when you finally notice them? They’ve already built a kingdom under your skin. We treat them like enemies. But maybe they’re teachers. Maybe they’re asking: ‘Why are you so damp? Why do you live like this?’
Terbinafine kills. But dryness? Dryness remembers. Dryness outlives. Dryness is the only cure that never forgets.
Ryan Everhart
November 18, 2025 AT 18:47So let me get this straight. You spent 800 words explaining that you need to dry your feet and not wear the same socks for a week… and this is groundbreaking? I’m shocked. The CDC really needs to fund this research. Next up: ‘Water is Wet: A Comprehensive Guide to Not Getting Soaked.’
David Barry
November 19, 2025 AT 21:31Let’s not romanticize this. Fungal infections are not ‘philosophical lessons.’ They’re inconvenient, embarrassing, and sometimes dangerous. The fact that we’re still using 1970s antifungals while Big Pharma chases billion-dollar cancer drugs is a failure of priorities. The WHO listing? Good. But it’s not enough. We need mandatory antifungal stewardship in hospitals, subsidized topical treatments for low-income communities, and real-time genomic surveillance for resistant strains. This isn’t about ‘being dry’-it’s about systemic neglect. And the fact that you’re calling it ‘boring’ just proves how little society cares until it’s their feet.
Alyssa Lopez
November 20, 2025 AT 20:18USA has the best medical tech in the world and we're still dealing with this? My cousin got athlete’s foot from a hotel in Bali and now she’s got a 3-month prescription. We need stricter border controls on fungal spores. Also, why is fluconazole still the go-to? It’s like using a typewriter in 2024. We need AI diagnostics and drone-delivered antifungals. This is embarrassing.
Alex Ramos
November 21, 2025 AT 02:27OMG YES. I had jock itch for 6 months. Tried everything. Then I started using miconazole powder in my socks AND my underwear. AND I changed my underwear midday if I sweated. AND I stopped wearing tight jeans. And guess what? Gone in 10 days. Also, I use a UV shoe sanitizer now. It’s $30 on Amazon. Life changed. 🙌
edgar popa
November 22, 2025 AT 14:39terbinafine ftw. i used it for 2 weeks and it never came back. just dry your feet. that’s it.
Benjamin Stöffler
November 22, 2025 AT 17:43And yet, here we are-still blaming the patient for not being ‘clean enough.’ The real failure isn’t the fungus. It’s the medical system that treats fungal infections as ‘minor’ while ignoring the social determinants: lack of access to clean water, shared housing, inadequate footwear, and the stigma that makes people hide their symptoms until they’re septic. Dryness isn’t a lifestyle tip-it’s a human right. And until we treat it that way, we’re not curing infections-we’re just managing shame.