IBD Biologics Explained: Anti-TNF, Anti-Integrin, and IL-12/23 Inhibitors for Crohn's and Colitis
 Jan, 26 2026
Jan, 26 2026
When you're living with Crohn's disease or ulcerative colitis, daily life can feel like a constant battle. Fatigue, pain, frequent bathroom trips - it’s exhausting. For many, standard treatments like steroids or immunomodulators just don’t cut it anymore. That’s where IBD biologics come in. These aren’t your ordinary pills. They’re precision-targeted drugs designed to calm down the immune system’s attack on your gut. And in the last 25 years, they’ve changed everything for millions of people.
What Are IBD Biologics?
IBD biologics are made from living cells, not chemicals. Think of them as lab-grown versions of proteins your body naturally produces to regulate inflammation. Instead of broadly suppressing your immune system like steroids do, these drugs zero in on specific troublemakers - molecules that are driving the inflammation in your intestines.
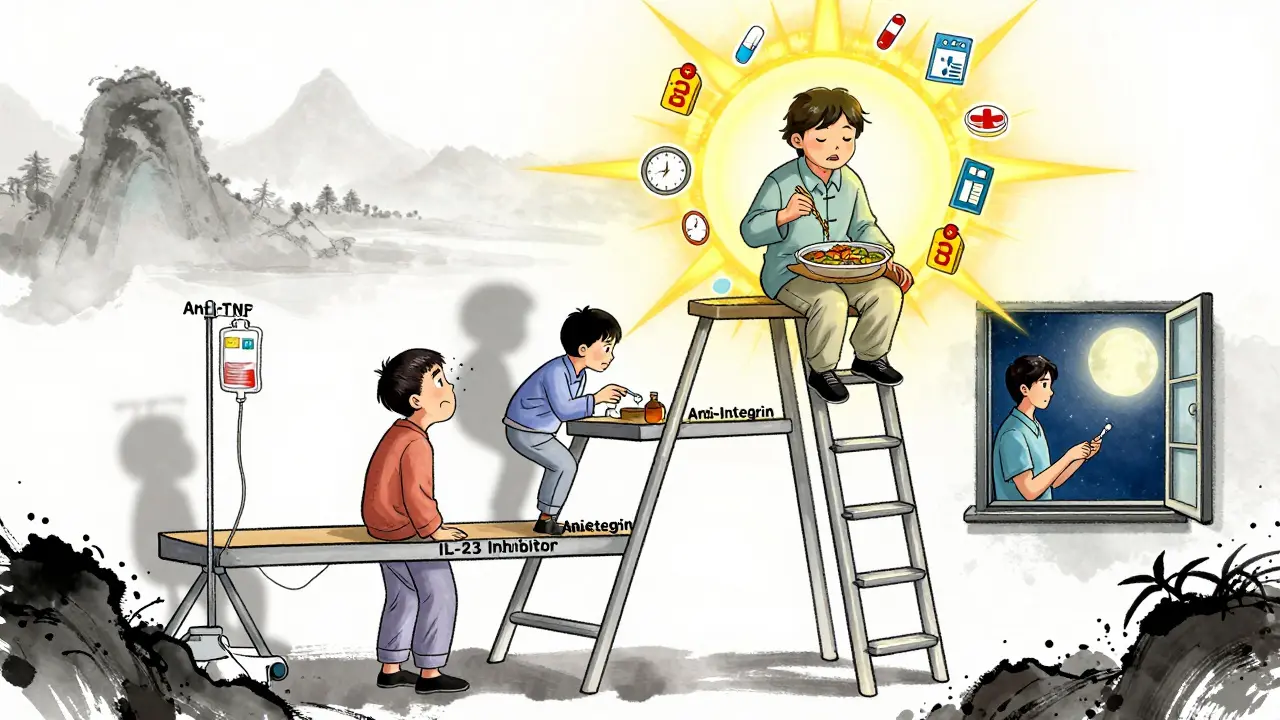
There are three main types you’ll hear about: anti-TNF, anti-integrin, and IL-12/23 inhibitors. Each works differently. And choosing the right one isn’t just about which one works best - it’s about what works best for you.
Anti-TNF Inhibitors: The First Wave
Anti-TNF drugs were the pioneers. Infliximab (Remicade) hit the market in 1998 and was the first biologic approved for Crohn’s. It quickly proved it could shut down inflammation when nothing else could. Today, this class includes infliximab, adalimumab (Humira), golimumab (Simponi), and certolizumab pegol (Cimzia).
They block tumor necrosis factor-alpha (TNF-α), a key signaling molecule that tells your immune system to attack your gut lining. For many, the results are dramatic. Studies show up to 70% of patients see symptom improvement within weeks.
But there’s a trade-off. Because these drugs affect the whole body, they carry higher risks. Serious infections - like tuberculosis or fungal infections - are more common. There’s also a small but real risk of lymphoma or other cancers. The FDA requires special monitoring programs (REMS) for all anti-TNFs.
Administration varies. Infliximab is given through an IV, usually at a clinic every 8 weeks after initial doses. It takes about 2-4 hours per session. Adalimumab is a self-injected shot every other week. Many patients prefer the convenience of injections - but injection site reactions (redness, itching, pain) happen in up to 30% of users.
Anti-Integrin Therapies: Targeting the Gut Only
If you’re worried about systemic side effects, vedolizumab (Entyvio) might be the better fit. It’s an anti-integrin drug that works differently. Instead of blocking a protein everywhere in the body, it only stops immune cells from entering the gut. Think of it like a bouncer at a club - it lets immune cells in everywhere else, but says “no entry” to the intestines.
This selective action means fewer infections, no increased cancer risk, and no risk of rare brain conditions like PML (which can happen with natalizumab, another integrin blocker no longer used for IBD). That’s why doctors often recommend vedolizumab for patients with a history of MS, TB, or those who’ve had bad reactions to anti-TNFs.
The catch? It’s slower. While anti-TNFs can start working in 2-4 weeks, vedolizumab often takes 6-10 weeks. Many patients report frustration during this waiting period. But once it kicks in, the results are steady. In patient surveys, 72% say it’s effective, and only 18% report side effects - the lowest rate among biologics.
Vedolizumab is given as an IV infusion every 8 weeks, same as infliximab. But unlike infliximab, it doesn’t cause infusion reactions as often. Still, the clinic visits add up - and for some, the travel and time make it hard to stick with long-term.
IL-12/23 and IL-23 Inhibitors: The New Generation
The newest class of IBD biologics targets interleukins - specifically IL-12 and IL-23, two cytokines involved in chronic gut inflammation. Ustekinumab (Stelara) was the first, approved for Crohn’s in 2016 and UC in 2019. It blocks both IL-12 and IL-23. Then came risankizumab (Skyrizi) and mirikizumab (Omvoh), which block only IL-23 - and they’re showing even better results.
Risankizumab got FDA approval for ulcerative colitis in June 2024, making it the first IL-23 inhibitor approved for both Crohn’s and UC. In clinical trials, nearly 30% of patients reached clinical remission after one year - more than double the placebo rate. And the safety profile? Cleaner than anti-TNFs. Fewer infections. No black box warnings. No need for REMS programs.
Both risankizumab and mirikizumab are self-injected, usually every 8-12 weeks. That’s less frequent than Humira. Many patients appreciate the balance: good efficacy, low side effects, and fewer injections.
Ustekinumab is still widely used, especially for patients who also have psoriasis - since it helps both conditions. But for pure IBD, the newer IL-23 blockers are quickly becoming the preferred option for many gastroenterologists.
Which One Works Best?
There’s no single “best” biologic. But data can help guide decisions.
In patients who’ve never tried a biologic before (bio-naive), infliximab has the strongest evidence for inducing remission - especially in moderate to severe ulcerative colitis. One meta-analysis found it was nearly twice as effective as adalimumab in getting patients into remission. For mucosal healing (actual repair of the gut lining), infliximab again leads the pack.
But here’s the twist: in real life, many patients choose adalimumab over infliximab simply because it’s easier. No clinic visits. No IV lines. Just a shot at home. And for mild-to-moderate disease, the slight edge in efficacy might not matter as much as convenience.
Vedolizumab doesn’t win on speed, but it wins on safety. Patients with a history of infections, TB, or neurological issues often do better on it. And in long-term studies, it’s linked to fewer hospitalizations than anti-TNFs.
For those who’ve tried one biologic and it stopped working, switching to a different class - say, from an anti-TNF to an IL-23 inhibitor - often brings back control. That’s why many doctors now think of biologics as a ladder: try one, if it fails, move to the next class, not just another drug in the same class.
Cost and Access: The Hidden Battle
These drugs aren’t cheap. A single dose of vedolizumab can cost $5,500. Ustekinumab? Around $7,200. Even with insurance, co-pays can hit $1,000 a month. That’s why manufacturer assistance programs are critical. Janssen, AbbVie, and Takeda all offer programs that reduce out-of-pocket costs to $0-$5 for eligible patients.
Biosimilars - cheaper copies of older biologics like infliximab and adalimumab - have cut prices by 15-30% since 2016. But not all insurers cover them automatically. Some still push the brand-name versions, even when the biosimilar is just as safe and effective.
And then there’s the time cost. Infusion therapies mean taking off half a day every 8 weeks. For working parents, people in rural areas, or those with mobility issues, that’s a huge burden. One Reddit user wrote: “Remicade worked within two weeks - but the 8-hour round trip every month? Unsustainable.”
Meanwhile, self-injectables require training, anxiety management, and steady hands. About 22% of patients need counseling to overcome injection fear.
What Patients Actually Say
On patient forums like MyIBDTeam and Reddit, the stories are raw and real.
“Switched from Humira to Entyvio after 5 years - no more weekly injections, but had to wait 10 weeks for full effect. That was brutal.”
“Remicade saved my life. I went from 15 bathroom trips a day to 2. But I hate the IVs.”
“Skyrizi? I got my first shot in December. By February, I was eating solid food again. No side effects. I’m not scared anymore.”
Common themes? Effectiveness is king - 78% of patients rank it above convenience. But 63% would switch to avoid infusions. And nearly half say cost is still a barrier, even with insurance.
What’s Next?
The future of IBD treatment is personalization. Researchers are now testing biomarkers - blood tests or stool markers - to predict who will respond to which drug. Trials like RHEA and VEGA are comparing biologics head-to-head, something we’ve lacked for years.
New drugs are coming. Etrolizumab, another gut-selective integrin blocker, is in late-stage trials. Mirikizumab is being tested for Crohn’s. And oral biologics? Those are still a few years off, but they’re on the horizon.
By 2030, experts predict 60% of moderate-to-severe IBD patients will be on biologics. But access remains uneven. One in four patients still report insurance denials. And long-term data on newer drugs like risankizumab? Still being collected.
The goal isn’t just to control symptoms. It’s to heal the gut, avoid surgery, and let people live full lives. For many, biologics have made that possible. The challenge now is making sure everyone who needs them can get them - without breaking the bank or burning out from clinic visits.
Key Takeaways
- Anti-TNFs (infliximab, Humira) work fast and are powerful, but carry higher infection and cancer risks.
- Vedolizumab is gut-specific, safer for long-term use, but slower to work - ideal for patients with infection or neurological risks.
- IL-23 inhibitors (Skyrizi, Omvoh) are the newest, safest, and most effective for many - now approved for both Crohn’s and UC.
- Cost and access are major hurdles; biosimilars and manufacturer programs can help reduce financial burden.
- Switching between biologic classes often works better than switching within the same class.
Frequently Asked Questions
How long does it take for IBD biologics to start working?
It varies by drug. Anti-TNFs like infliximab and Humira often start working in 2-4 weeks. Vedolizumab takes longer - 6 to 10 weeks for noticeable improvement. IL-23 inhibitors like Skyrizi usually show effects within 4-8 weeks, with full benefit by 12-16 weeks. Patience is key, but if you see no change after 12 weeks, talk to your doctor about adjusting your plan.
Can I stop taking biologics if I feel better?
Stopping biologics is risky. Even if you’re in remission, stopping often leads to flare-ups - and sometimes, the drug won’t work as well if you restart it. Some patients do successfully taper off under close supervision, but it’s rare. Most experts recommend staying on maintenance therapy long-term to keep inflammation under control and prevent complications like strictures or cancer.
Do biologics increase my risk of cancer?
Anti-TNF drugs carry a small increased risk of lymphoma and skin cancer. That’s why regular skin checks and avoiding excessive sun are recommended. IL-23 inhibitors like Skyrizi and IL-12/23 inhibitors like Stelara don’t show the same cancer risk in studies so far. Vedolizumab has no known cancer risk. Always discuss your personal risk factors - like family history or previous skin cancers - with your doctor before starting.
What if my biologic stops working?
Loss of response is common, especially with anti-TNFs. It’s often due to your body making antibodies against the drug. Solutions include increasing the dose, shortening the interval between doses, or adding an immunomodulator like azathioprine. If that doesn’t help, switching to a biologic from a different class - like from Humira to Skyrizi - is often the next step. Most patients respond well to a switch.
Can I get vaccinated while on biologics?
Yes - but timing matters. You should get all routine vaccines (flu, pneumonia, shingles, COVID-19) before starting a biologic. Live vaccines (like MMR or yellow fever) are not safe once you’re on treatment. Inactivated vaccines are fine and strongly recommended. Ask your doctor for a vaccination checklist before your first infusion or injection.

Conor Murphy
January 28, 2026 AT 01:46Just wanted to say thank you for this. I’ve been on Entyvio for 2 years now and honestly? It gave me my life back. No more panic attacks before leaving the house. No more counting minutes until the next bathroom run. I know it’s slow but trust me, it’s worth the wait. 🙏
Paul Taylor
January 29, 2026 AT 18:09I switched from Humira to Skyrizi last year and wow what a difference I was having constant joint pain and fatigue and honestly felt like I was dying slowly then after my third shot I started eating again like normal food not just mashed potatoes and broth and I haven’t been to the ER in 11 months and my doctor said my colon looks better than some 20 year olds
Patrick Merrell
January 31, 2026 AT 11:08Anyone else notice how the pharmaceutical companies push the new expensive drugs like Skyrizi like they’re magic bullets while ignoring the fact that biosimilars work just as well for 80% of people? 🤨 This isn’t medicine it’s a profit scheme. They don’t care if you can afford it they just want you hooked on the latest $7k/month wonder drug.
Conor Flannelly
February 2, 2026 AT 07:22There’s something deeply human about how these drugs don’t just treat symptoms but restore dignity. I remember sitting in that infusion chair for the first time thinking I’m not just getting medicine I’m getting back the ability to hug my kid without worrying I’ll collapse. The science is impressive but the real miracle is the quiet moments after treatment when you realize you can breathe again. We talk about efficacy rates and remission but we forget the weight of a normal day.
Harry Henderson
February 2, 2026 AT 18:01Stop being so nice to these drug companies. If you’re on an anti-TNF and you’re not in remission after 8 weeks you’re wasting your time. Switch. Now. Don’t wait for your doctor to tell you. You know your body better than they do. I was on Remicade for 3 years and it stopped working. I switched to Skyrizi and boom. No more flares. No more hospital visits. No more begging for pain meds. If you’re not aggressive about your treatment you’re letting IBD win.
astrid cook
February 3, 2026 AT 22:50Why do people keep saying vedolizumab is safe? My cousin got a fungal infection from it and ended up in the ICU for 3 weeks. And don’t even get me started on the cost. I work two jobs and still can’t afford the co-pay. They tell you to apply for assistance programs but the paperwork is a nightmare. This isn’t healthcare. It’s a rigged game.
Andrew Clausen
February 5, 2026 AT 03:29Correction: risankizumab was approved for ulcerative colitis in June 2024 but not for Crohn’s disease as stated. The FDA label explicitly restricts it to UC. Mirikizumab is approved for UC but not yet for Crohn’s. The post contains a factual error. Precision matters when discussing treatment options. Please update.
Anjula Jyala
February 5, 2026 AT 22:36IL-23 inhibition is the future because it targets the Th17 pathway which is the dominant inflammatory axis in IBD not just TNF. The cytokine cascade is more complex than the old paradigm suggests. Biosimilars are not equivalent in pharmacokinetics due to glycosylation patterns and immunogenicity profiles. You need biomarker-guided therapy not trial and error. JAK inhibitors are coming but they’re not biologics so they’re irrelevant here.
Kirstin Santiago
February 7, 2026 AT 10:15I started Skyrizi last month and honestly I’m just taking it one day at a time. Some days I feel great other days I’m still tired but I’m trying to be patient. My mom said I should’ve switched sooner but I’m just glad I’m finally on something that feels like it might work. Thanks for sharing this info it helped me feel less alone.
Kathy McDaniel
February 8, 2026 AT 06:19my first shot was a disaster i cried the whole time but now i do it myself and its kinda chill? like giving myself a little hug with a needle lmao
Marian Gilan
February 9, 2026 AT 14:18They’re watching us. The biologics? They’re not just drugs. They’re tracking devices. Every infusion. Every injection. Every blood test. They’re gathering data on your immune system. Why do you think the FDA is so eager to approve new ones? It’s not about healing. It’s about control. You think you’re getting better? You’re just becoming more dependent. Wake up.