Osteoarthritis of the Hip: How Weight Loss Can Preserve Your Joint and Reduce Pain
 Jan, 28 2026
Jan, 28 2026
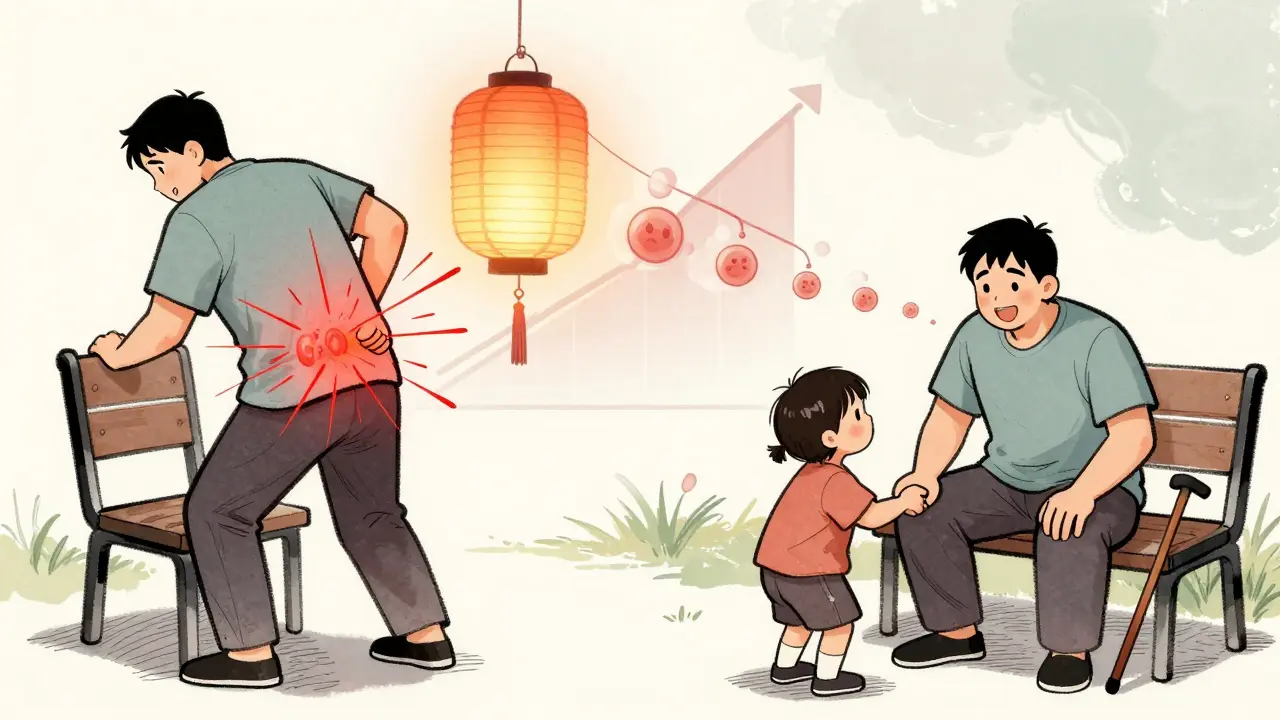
When your hip starts hurting every time you stand up, walk, or even roll over in bed, it’s easy to assume surgery is the only way out. But what if the key to relief isn’t a scalpel - it’s your diet and movement? For many people with hip osteoarthritis (OA), losing weight isn’t just about looking better - it’s one of the most powerful, science-backed ways to slow joint damage and feel like yourself again.
What Hip Osteoarthritis Really Does to Your Body
Hip osteoarthritis isn’t just "wear and tear." It’s an active process where the cartilage cushioning your hip joint breaks down, bones rub against each other, and inflammation sets in. This leads to pain that gets worse with activity, stiffness after sitting for too long, and a feeling that your leg doesn’t move the way it used to. The pain can spread to your groin, thigh, or even your knee. And if you’re carrying extra weight, every step you take puts 3 to 6 times your body weight through that joint.
According to the Johns Hopkins Arthritis Center, hip OA is one of the most common causes of disability in adults over 50. And while it’s often lumped together with knee OA, the two aren’t the same. Your hip is a ball-and-socket joint designed for stability, not flexibility. That means the forces it handles are different - and so is how it responds to weight loss.
Why Weight Loss Isn’t Just Helpful - It’s Necessary
For years, doctors told people with knee OA to lose weight because the data was clear: every pound lost meant four pounds less pressure on the knee. But when it came to the hip, the message got fuzzy. Some studies said it worked. Others said it didn’t. Then came the 2024 Nature study - the largest and most detailed look at weight loss and hip OA to date.
The study followed 65-year-old adults, mostly women with obesity (BMI ≥30), who lost weight over 18 weeks. The results were clear: the more weight people lost, the better their symptoms got. Those who lost more than 10% of their body weight saw a 31% improvement in their quality of life - the biggest jump of any symptom group. Pain dropped. Stiffness eased. Walking got easier. Even the ability to do things like climb stairs or play with grandchildren improved.
That’s not a small win. It’s life-changing. And it’s not just about feeling better - it’s about protecting your joint. Less weight means less mechanical stress on the cartilage. Less inflammation from fat tissue means less chemical damage to the joint. In other words, losing weight doesn’t just mask the pain - it helps your hip heal.
The 10% Rule: Why More Is Better
You’ve probably heard "lose 5% of your weight" as the magic number for joint pain. That advice mostly comes from knee OA studies. But for hips, the data tells a different story.
The 2024 Nature study found that people who lost 5-7% saw modest improvements. But those who lost 10% or more had dramatic, clinically meaningful changes across all measures - pain, function, stiffness, and daily living. Even better, there was no extra benefit from losing 20% vs. 10%. That means 10% is the sweet spot: enough to make a real difference, without needing to become a different person.
For someone who weighs 200 pounds, that’s 20 pounds. For someone who weighs 160, it’s 16. It’s not about extreme dieting. It’s about consistent, sustainable change.
Why Some Studies Say Weight Loss Doesn’t Help the Hip
So why does the NEJM Journal Watch say, "Osteoarthritis of the Hips Is Unaffected by Weight Loss"? Because of a 2023 trial that compared a very-low-calorie diet (VLCD) plus exercise to exercise alone.
At six months, the VLCD group had lost more weight - 8.5% more - but their hip pain scores didn’t improve any more than the exercise-only group. That’s where the confusion came from. But here’s the catch: the real benefits didn’t show up until 12 months. By then, the VLCD group had better pain scores, better function, and higher overall satisfaction. The body takes time to respond.
This is critical. If you quit after three months because you don’t feel better, you’re missing the point. Weight loss for hip OA isn’t a quick fix. It’s a long-term repair job. The joint doesn’t heal overnight. But over time, less pressure + less inflammation = less pain and slower degeneration.
What Actually Works: The Proven Approach
The Osteoarthritis Healthy Weight For Life (OAHWFL) program, developed in Australia and New Zealand, gives us the clearest blueprint. It’s not just "eat less, move more." It’s structured, supported, and science-backed.
- 18 weeks of focused weight loss: Combines low-carb, high-protein eating with daily movement tailored for hip OA.
- Exercise that protects the joint: Not running or jumping. Think swimming, cycling, resistance training with bands or light weights, and balance work.
- Weekly coaching: Whether in person or via telehealth, having someone guide you makes a huge difference in sticking with it.
- Maintenance phase: After 18 weeks, you shift from losing weight to keeping it off - which is where most programs fail.
A 2012 study of 35 people with hip OA who followed a similar 8-month plan saw a 32.6% improvement in physical function. That’s not a 10% gain. That’s a full third better. People went from struggling to get out of a chair to walking without pain.
What to Avoid
Not all weight loss plans are created equal - especially when you have hip OA.
- High-impact workouts: Running, jumping, or step aerobics can make hip pain worse. Swap them for low-impact options.
- Extreme diets: Keto, juice cleanses, or fasting for weeks can lead to muscle loss - and you need muscle to support your hip.
- Ignoring strength training: Strong glutes, quads, and core muscles act like shock absorbers for your hip. Skip them, and you’re relying on bone-on-bone contact.
- Waiting for pain to disappear before moving: Movement is medicine. Even gentle walking or water aerobics helps reduce stiffness and improve circulation to the joint.
When Weight Loss Isn’t Enough
Some people do everything right - lose 10%, exercise regularly, eat well - and still have pain. That doesn’t mean they failed. It means they need more.
Weight loss is the foundation. But for lasting relief, you need to combine it with:
- Physical therapy: A PT can teach you how to move without aggravating your hip.
- Heat, ice, and massage: Simple tools that reduce inflammation and ease stiffness.
- Assistive devices: A cane or walker used correctly can cut pressure on the hip by up to 25%.
- Medications: NSAIDs like ibuprofen help with flare-ups, but they’re not long-term solutions. The American College of Rheumatology recommends them only for short-term use.
Drugs like semaglutide (Wegovy) or tirzepatide (Zepbound) are now approved for weight loss in people with obesity and OA. But they’re not first-line. They’re for those who’ve tried lifestyle changes for at least six months and still haven’t reached their goal.

Real People, Real Results
Take Sarah, 62, from Bristol. She had hip OA for five years. Walking to the bus stop left her in tears. Her doctor told her to lose weight - but she didn’t know how. She joined a local program that matched the OAHWFL model. Over six months, she lost 18 pounds. Not because she starved herself. Because she ate more protein, cut sugary drinks, and walked 20 minutes a day.
Today, she walks her dog without pain. She plays with her grandkids. She doesn’t need a cane anymore. She didn’t have surgery. She didn’t take pills long-term. She just changed how she lived.
What You Can Do Today
You don’t need a fancy program to start. Here’s your simple first step:
- Measure your weight. Write it down.
- Set a 10% goal. If you weigh 180 lbs, aim for 162.
- Swap one sugary drink a day for water or tea. That’s 200-300 calories gone.
- Walk for 15 minutes, three times this week. No need to push through pain - just move.
- Call your doctor or a physiotherapist. Ask about a joint-friendly exercise plan.
That’s it. No extremes. No magic pills. Just small, consistent actions that add up.
Weight loss won’t erase hip osteoarthritis. But it can stop it from getting worse. It can give you back your mobility. It can delay - or even prevent - surgery. And that’s not just hope. That’s science.
Is Surgery the Only Option Left?
Not if you act now. Studies show that people who lose 10% or more before joint replacement have better outcomes, faster recovery, and lower risk of complications. Weight loss isn’t just a backup plan - it’s part of the treatment plan, even if surgery is in your future.
And if you’re not ready for surgery? Losing weight might be the only thing standing between you and a lifetime of pain.

Laia Freeman
January 29, 2026 AT 05:16This literally changed my life-I lost 12 lbs in 3 months, swapped soda for sparkling water, and now I can play with my grandkids without crying after 5 minutes. I didn’t even need surgery!!
Andy Steenberge
January 30, 2026 AT 02:58The science here is rock-solid. Weight loss doesn’t just reduce mechanical load-it lowers systemic inflammation, which is a huge driver of OA progression. The 10% threshold is critical because fat tissue isn’t inert; it’s metabolically active, secreting cytokines that accelerate cartilage degradation. Most people underestimate how much this biochemical shift matters. And yes, it’s not about aesthetics-it’s about preserving function. This isn’t a diet tip. It’s a joint preservation protocol.
Frank Declemij
January 30, 2026 AT 17:21Agreed. The 2024 Nature study is the most compelling evidence we’ve had. The fact that 10% was the sweet spot and no extra benefit came from 20% is huge. It means the goal is achievable. No need for extremes. Just consistency. This should be standard advice from every ortho clinic.
DHARMAN CHELLANI
January 31, 2026 AT 06:11Yeah right, lose 10% and your hip magically heals. What about the people who lose 20% and still need a replacement? This is just corporate wellness fluff dressed up as science. The real fix is surgery. Everything else is placebo with extra steps.
Alex Flores Gomez
January 31, 2026 AT 08:30Interesting how they cite an Australian program like it’s gospel. Meanwhile, in the U.S., we’ve got actual clinical trials from Mayo and Cleveland Clinic that show mixed results. This feels like a PR piece for some wellness influencer’s eBook. Also, why is everyone ignoring the role of insulin resistance? No mention of that? Typical.
rajaneesh s rajan
January 31, 2026 AT 17:28Look, I get it. Lose weight, feel better. But let’s be real-most people with hip OA are older, sedentary, maybe on meds, maybe depressed. Telling them to ‘swap one soda’ is like telling a drowning man to ‘try breathing slower.’ It’s not that the advice is wrong-it’s that the system doesn’t support it. Who’s gonna coach them? Who’s gonna pay for PT? Who’s gonna help them cook protein meals when they’re on Social Security? This article feels like a luxury.
Pawan Kumar
February 1, 2026 AT 22:47Did you know that Big Pharma secretly funded this study? The same companies that sell joint replacements also own the weight-loss supplement market. The 10% rule is a distraction. Real solutions involve gene therapy and stem cells-things the FDA suppresses because they’re not profitable. You think this is about health? It’s about control.
kabir das
February 2, 2026 AT 09:02I’ve been trying for 14 months!!! I did everything!!! Keto!!! Daily walks!!! Protein shakes!!! And my hip still screams at me every morning!!! Why is no one listening??? I feel so alone in this!!!
paul walker
February 4, 2026 AT 09:02Hey, I’m right there with you-been there, cried in the shower over it too. But I started with just 10 minutes of water aerobics 3x a week and swapped out one snack for nuts. Took 8 months, but I lost 14 lbs. Pain didn’t vanish overnight, but it got quieter. You’re not alone. Small steps. Keep going.