Statin-Induced Muscle Pain: Understanding Myalgia and Myositis
 Nov, 24 2025
Nov, 24 2025
Statin Muscle Pain Risk Assessment
This tool helps assess your risk of statin-induced muscle conditions based on your symptoms, medical history, and test results. Results are based on clinical guidelines from the article "Statin-Induced Muscle Pain: Understanding Myalgia and Myositis".
Symptom Assessment
Risk Factors
Test Results
0%
When you start taking a statin to lower your cholesterol, you expect better heart health-not constant aches, weakness, or fatigue. But for many people, muscle pain becomes the unexpected price of taking these common drugs. Statin-induced muscle pain isn’t just a nuisance. It can be a sign of something more serious: myalgia, myositis, or even immune-mediated necrotizing myopathy. Understanding the difference matters because how you respond could change your long-term health.
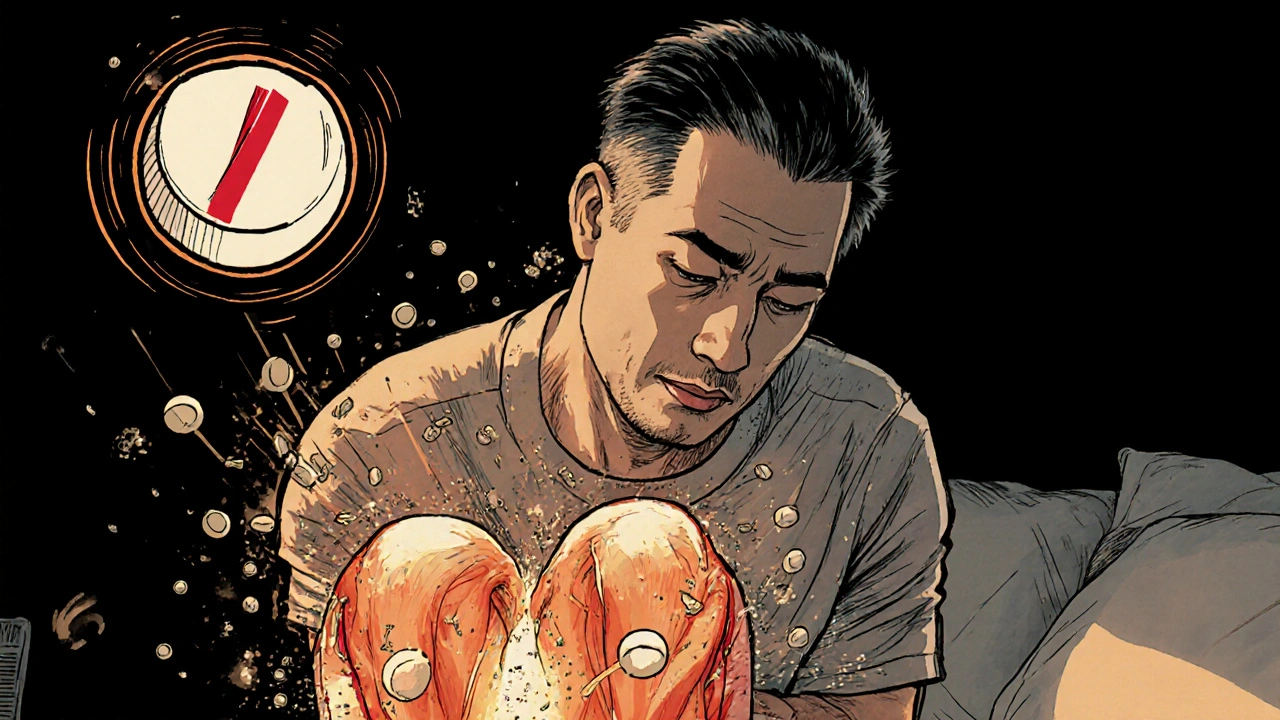
What’s Really Going On in Your Muscles?
Statins work by blocking HMG-CoA reductase, an enzyme your liver uses to make cholesterol. But that same enzyme is also involved in making other vital compounds in your muscles, like coenzyme Q10 (CoQ10) and proteins needed for energy production. When statins cut these off, your muscle cells start to struggle. Think of it like turning down the fuel to your car’s engine-you might still run, but you’ll sputter, feel weak, and eventually break down. CoQ10 levels can drop by up to 40% in people taking 40 mg of simvastatin daily. That means less ATP, the energy your muscles need to contract and recover. On top of that, statins disrupt how proteins are modified inside muscle cells, leading to calcium leaks that trigger enzymes that chew up muscle tissue. In some cases, your immune system even starts attacking your own muscles because it mistakes the HMG-CoA enzyme-now overproduced due to statin use-for a foreign invader.Myalgia: The Common, Often Misunderstood Pain
Most people who get muscle pain on statins have myalgia. It’s the most common form, affecting 10% to 29% of users. You feel soreness, stiffness, or cramps, usually in your thighs, shoulders, or lower back. But here’s the catch: your creatine kinase (CK) levels-the blood marker for muscle damage-are normal or only slightly elevated. That’s why many doctors dismiss it as "just aging" or "overexertion." But if the pain started after you began taking a statin, and it went away when you stopped, that’s not coincidence. It’s a signal. A 2014 JAMA Internal Medicine review found that nearly 30% of patients who stopped statins because of muscle pain saw their symptoms vanish within weeks. The problem? Many never get the chance to test that theory because their doctor doesn’t ask the right questions.Myositis: When Your Muscles Are Inflamed
Myositis is rarer but more serious. It happens in about 0.5% of statin users. Unlike myalgia, your CK levels rise significantly-10 to 40 times above normal. That means actual muscle inflammation and damage are happening. You might notice weakness when climbing stairs, lifting your arms, or getting up from a chair. Some people describe it as feeling like they’re carrying weights all day. A muscle biopsy is often needed to confirm it. The tissue shows signs of inflammation and damaged fibers. But here’s what many doctors miss: if your symptoms don’t improve after stopping the statin for 2-4 weeks, you’re not just dealing with simple myopathy. You might be developing something far more dangerous.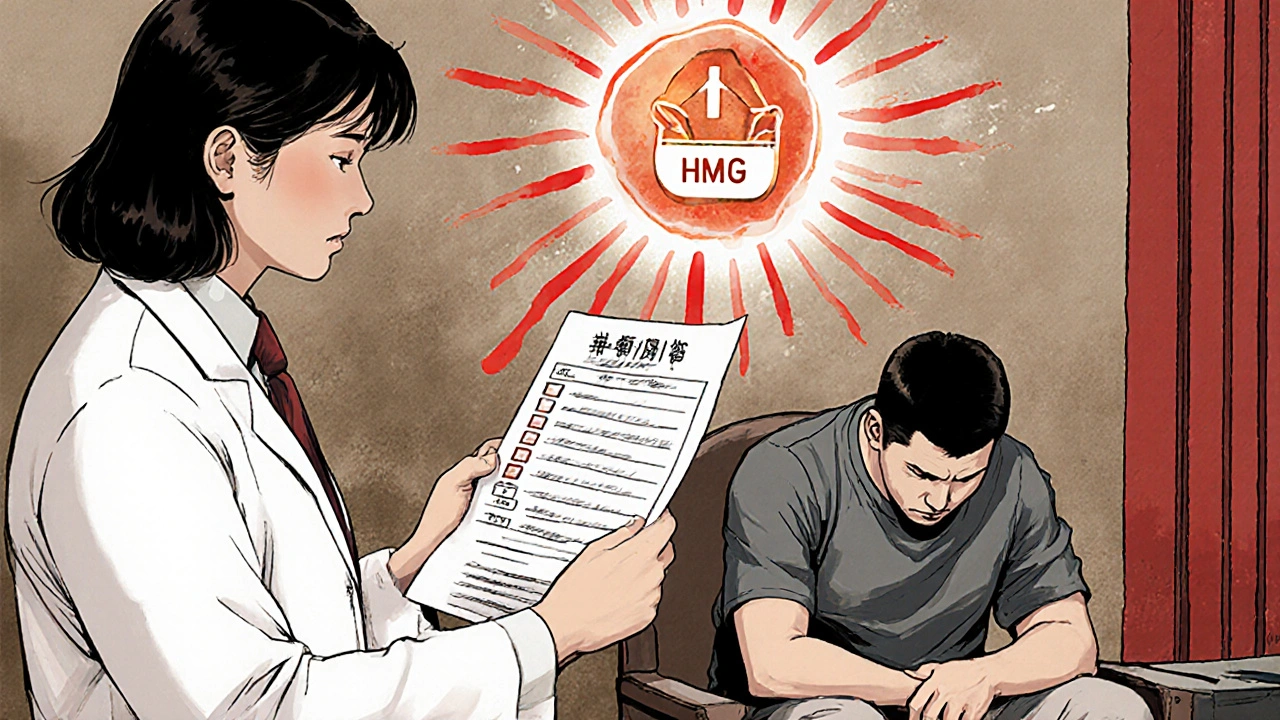
Immune-Mediated Necrotizing Myopathy: The Silent Threat
This is the most serious form, known as statin-associated autoimmune myopathy (SAAM) or anti-HMGCR myopathy. It affects only 2-3 in every 100,000 statin users, but it’s often misdiagnosed for months-or even years. People with SAAM don’t just feel sore. They get progressively weaker. The weakness is symmetrical, hitting the hips and shoulders first. CK levels often soar above 2,000 IU/L (normal is 30-200). Even after stopping the statin, symptoms don’t fade. In fact, half of patients still feel weak 6 to 12 months later. Why? Because your immune system has turned on your own muscle cells. Antibodies are attacking the HMG-CoA enzyme-exactly what the statin was meant to block. A 2018 review found that 70% of these patients carry a specific gene variant, HLA-DRB1*11:01, making them genetically vulnerable. What makes this so dangerous is the delay in diagnosis. On patient forums, 68% of SAAM cases were first mistaken for fibromyalgia or chronic fatigue. One Reddit user reported 18 months of worsening weakness before getting the right diagnosis. By then, he needed six months of IVIG therapy just to start recovering.Who’s at Risk-and Why?
Not everyone on statins gets muscle pain. But some groups are far more vulnerable. - Age: People over 50 are at higher risk, especially for SAAM. The immune system becomes more reactive with age. - Genetics: The SLCO1B1 gene variant rs4149056 increases simvastatin myopathy risk from 0.6% to 1.4%. This is especially common in people of European and Asian descent. - Race: African Americans have 1.8 times higher risk than Caucasians, likely due to genetic differences in how statins are transported into muscle cells. - Drug interactions: Taking statins with amiodarone, clarithromycin, or grapefruit juice can spike statin levels by 300-500%. That’s like doubling your dose without realizing it. - Low vitamin D: Deficiency is linked to worse muscle symptoms. Many statin users also have low vitamin D-it’s a double hit.What Should You Do If You Have Muscle Pain?
Don’t ignore it. Don’t assume it’s normal. Here’s what to do step by step:- Stop the statin. Not forever-just for 2-4 weeks. This is the first diagnostic test.
- Get a CK blood test. Normal? Probably myalgia. High? You need more testing.
- Check your thyroid and vitamin D. Both can mimic statin muscle pain.
- If pain persists beyond 4 weeks, ask for an anti-HMGCR antibody test. This is critical. If positive, you have SAAM.
- See a neuromuscular specialist. Not your GP. Someone who knows how to read muscle biopsies and interpret immune markers.

Josh Gonzales
November 25, 2025 AT 12:58Been on atorvastatin for 5 years no issues but my buddy dropped simvastatin and couldnt lift his coffee cup for 3 months. CK was through the roof. Doc said "its all in your head" until he got the anti-HMGCR test. Then it was IVIG and 6 months of hell. Bottom line dont ignore it. Get tested.
Emily Craig
November 26, 2025 AT 23:15YESSSS this is why i stopped statins after 2 weeks of feeling like i was dragged behind a truck for 30 miles. My doc laughed. I cried. Then i went to a rheumatologist who said "honey you dont have fibromyalgia you have SAAM". Took 8 months to feel human again. Your muscles are not optional.
katia dagenais
November 28, 2025 AT 21:52Oh so now its not just cholesterol youre saving but your muscles too? How noble. Meanwhile my cholesterol dropped 40 points and my heart stopped screaming. But sure lets all go on a witch hunt for HMGCR antibodies like its 2003 and we're chasing aliens. People are dying of heart attacks because they listened to Reddit instead of their cardiologist. CoQ10 supplements are a placebo with a fancy label. You want to feel better? Eat less sugar. Move more. Stop blaming drugs for your laziness.
Caroline Marchetta
November 30, 2025 AT 08:26So let me get this straight… you’re telling me that after 20 years of taking statins, my chronic fatigue, joint pain, and inability to climb stairs isn’t just "getting older"… it’s my immune system turning my muscles into confetti? And the doctor who told me to "just push through"… was he the same one who prescribed me this poison in the first place? How poetic. How tragic. How very, very corporate.
Jack Riley
December 1, 2025 AT 20:24Statins are the pharmaceutical equivalent of cutting the brake lines on your car and calling it "preventative maintenance." You don’t fix cholesterol by starving your mitochondria-you fix it by fixing your gut, your stress, your sleep, your damn diet. The body isn’t a machine you can tweak with a molecular wrench. It’s a symphony. And statins? They’re the guy smashing the cello because he thinks it’s too loud. Meanwhile the violinist (your muscles) is screaming.
And don’t even get me started on the HLA-DRB1*11:01 gene. That’s not a risk factor-it’s a death sentence written in DNA. You’re not a patient. You’re a genetic lottery ticket that lost.
And CoQ10? A Band-Aid on a severed artery. You think popping a pill fixes a system-wide sabotage? Please. The real drug isn’t statin-it’s denial. And the pharma companies? They’re the ones with the IV drip.
My uncle took simvastatin for 18 months. Walked into the ER with CK at 12,000. No muscle biopsy. No antibody test. Just "you’re old, rest up." He died of cardiac arrest two weeks later. They called it "natural causes." I called it murder by prescription.
And now they want us to believe that PCSK9 inhibitors are the answer? More expensive, less tested, same playbook. The system doesn’t want to fix this. It wants to monetize it. And we’re all just collateral damage with a prescription bottle.
So go ahead. Take your statin. Take your CoQ10. Take your denial. But don’t tell me it’s not a war. It’s a war. And your muscles are the front line.
Jefriady Dahri
December 2, 2025 AT 15:29Bro i was on rosuvastatin for 2 yrs and my legs felt like concrete. I stopped. 3 days later i could run again. No biopsy no nothing. Just listen to your body. Also vitamin d is 100% key. My levels were 18. Now i take 5k daily and feel like a new man 😊
Jacqueline Aslet
December 3, 2025 AT 12:43It is, of course, an unfortunate and deeply concerning phenomenon that the pharmacological intervention intended to mitigate cardiovascular risk may inadvertently precipitate a cascade of neuromuscular dysfunction. One cannot help but observe the profound dissonance between the clinical imperative to reduce LDL and the physiological toll exacted upon skeletal muscle integrity. The literature, while compelling, remains insufficiently integrated into primary care protocols, resulting in a lamentable diagnostic delay for a subset of patients who are, in effect, casualties of therapeutic overreach.
Valérie Siébert
December 3, 2025 AT 21:50OMG I had this!! I thought i was just lazy or had fibromyalgia but nooo it was SAAM!! I was so weak i couldnt open a jar and my doc was like "maybe try yoga". I cried in the parking lot. Then i found a neurologist who knew what HMGCR was and we did the test. Antibodies positive. IVIG. 6 months. Now i can lift my kids again. If you feel off on statins? GO TO A SPECIALIST. NOT YOUR GP. PLEASE.
Andrew Camacho
December 4, 2025 AT 12:09Let’s be real here-this whole statin thing is a $20 billion scam. You think the doctors don’t know this? They’re paid by pharma. They’re incentivized to keep you on it. The CK test? Useless. The antibody test? Too expensive. The biopsy? Too invasive. They’d rather you die of a heart attack than admit they gave you a drug that turns your muscles into Swiss cheese. And don’t even get me started on the genetic part-this isn’t science, it’s eugenics with a prescription pad. You’re not a patient. You’re a revenue stream.
And CoQ10? A joke. A placebo for people who still believe in magic pills. The real fix? Stop taking statins. Stop trusting doctors. Stop trusting the system. Your body is smarter than your pharmacist.
Karen Willie
December 6, 2025 AT 05:19Thank you for writing this. I’ve been afraid to speak up about my muscle pain because everyone says "statins save lives." But I’m 58, and I can’t carry groceries anymore. I finally stopped the simvastatin and got tested. Anti-HMGCR positive. I’m on prednisone now. It’s scary, but I’m getting stronger. You’re not alone. And your pain matters. Please, if you’re reading this and feel off-don’t wait. Push for the test. You deserve to move without pain.
Arup Kuri
December 6, 2025 AT 08:54Statins are a government mind control program disguised as medicine. They lower cholesterol but also lower your will to live. They make you weak so you stay home and watch TV. The HMGCR antibody? That’s not natural-that’s engineered. They want you dependent. They want you on pills. They want you scared. Your muscles are a warning. Listen. Stop the poison. Eat meat. Lift weights. Don’t trust the FDA. Don’t trust your doctor. The truth is hidden.
Josh Gonzales
December 7, 2025 AT 12:15Just had a patient come in yesterday. Same story. Stopped statin. CK dropped. Antibodies negative. Back to hiking in 3 weeks. Doc says it’s myalgia. I say it’s a lesson. Listen to your body. Test before you quit. But don’t let fear silence you.