Medication Strength Verification: How to Confirm Dosage Accuracy and Avoid Dangerous Errors
When you pick up a prescription, medication strength verification, the process of confirming the exact dose and form of a drug matches what was prescribed. Also known as drug dosage validation, it’s not just a pharmacy formality—it’s your last line of defense against a dangerous mistake. A 10mg pill can look identical to a 50mg pill. A generic version might have a different shape or color. And if you’re taking multiple meds, mixing them up is easier than you think.
Medication strength verification matters because errors happen more often than you’d guess. The FDA reports that over 1.3 million medication errors occur each year in the U.S. alone, and many are tied to confusion over dosage strength. It’s not always the pharmacist’s fault—sometimes the label fades, the bottle gets swapped, or the prescription gets misread. That’s why you need to know how to check for yourself. Look at the pill’s imprint code, compare it to the pharmacy’s printed label, and match the strength listed on the bottle to what your doctor ordered. If something feels off, ask. Pharmacists expect this question. In fact, a 2022 study in the Journal of Patient Safety found that patients who asked about dosage were 70% less likely to take an incorrect amount.
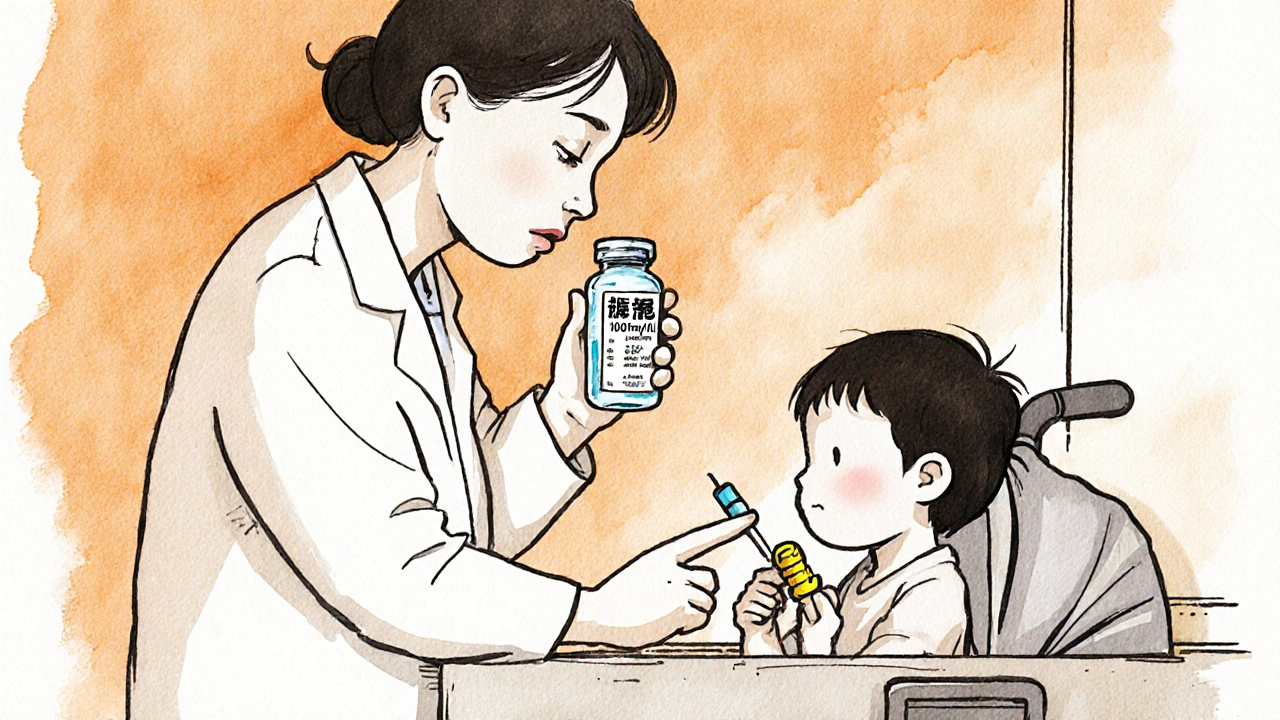
This isn’t just about pills. It applies to liquids, patches, injections, and even over-the-counter meds. A liquid antibiotic labeled 5mg/mL might be confused with one labeled 10mg/mL if you don’t check the unit. A fentanyl patch with 25mcg/hour is dangerously strong compared to a 12mcg/hour patch—same size, totally different effect. That’s why pill identification, using visual and coded markers to confirm a medication’s identity and strength. Also known as tablet verification, it’s a critical tool for anyone managing chronic conditions. Tools like the FDA’s National Library of Medicine’s Pillbox database or a simple phone app can help you match an unknown pill to its correct name and dose. And if you’re on high-risk meds like warfarin, insulin, or opioids, double-checking every time isn’t paranoia—it’s survival.
Also, don’t overlook pharmacy verification, the process where pharmacists cross-check prescriptions, dosages, and patient history to catch errors before they reach you. Also known as medication reconciliation, it’s a standard practice—but only if you give them full information. Tell your pharmacist about every supplement, herb, or OTC drug you take. They can spot interactions or strength mismatches you might miss. For example, if you’re on levothyroxine and start taking fiber supplements, your pharmacist should flag that timing matters. If you’re switching from brand to generic, they should confirm the bioequivalence isn’t compromised.
Medication strength verification isn’t a one-time task. It’s a habit. Every time you refill a prescription, even if it’s the same drug, check the pills. Compare them to the last batch. If they look different, ask why. Don’t assume the pharmacy got it right. Don’t assume the doctor changed nothing. And don’t ignore that little voice in your head that says, "This doesn’t feel right." That voice saved lives in the posts below—like the patient who caught a tenfold overdose in her statin dose, or the caregiver who noticed her mother’s antidepressant pills had changed color and refused to take them until it was cleared.
Below, you’ll find real stories and practical guides on how to spot dangerous mismatches, how to talk to your pharmacist without sounding suspicious, and how to use simple tools to verify your meds at home. Whether you’re managing chronic pain, heart disease, mental health, or just taking a new antibiotic, these posts give you the exact steps to stay safe. No fluff. No jargon. Just what works.