Pharmacy Double-Check: Why It Saves Lives and How to Get It Right
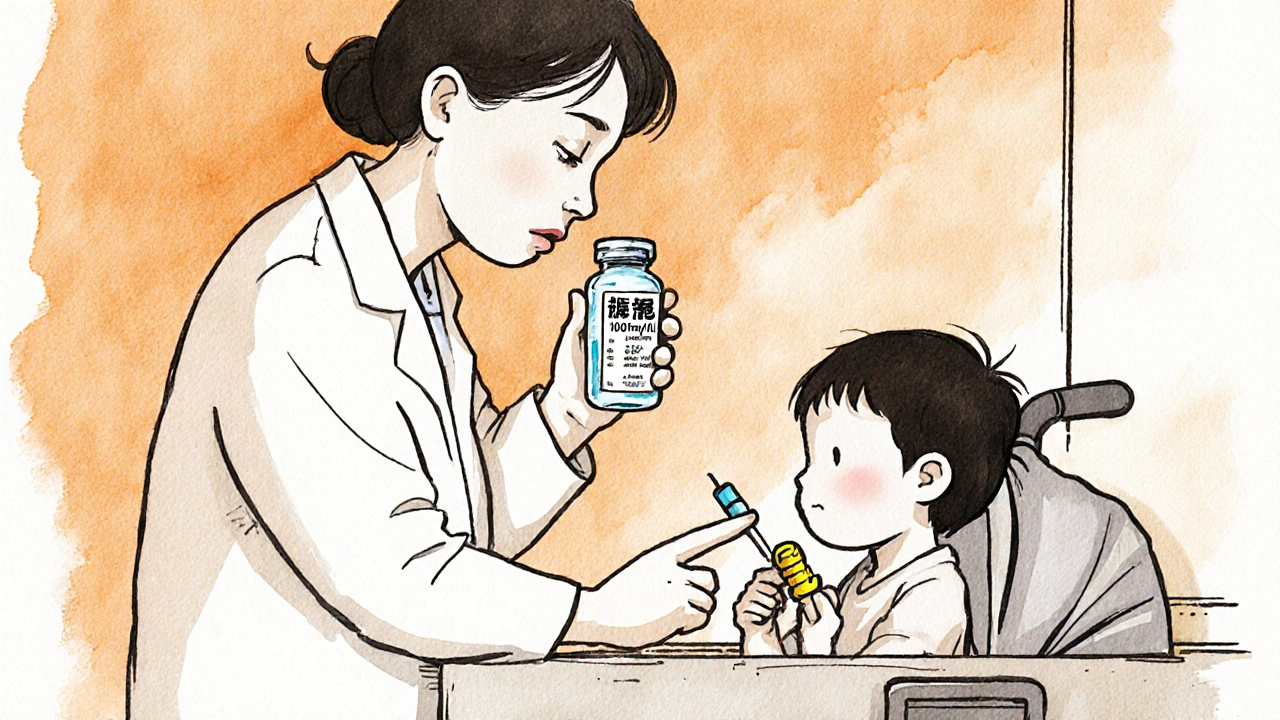
When you walk into a pharmacy, the person handing you your pills isn’t just filling a script—they’re part of a final safety line called a pharmacy double-check, a mandatory verification step where two trained professionals review a prescription before it’s dispensed. Also known as final verification, this step catches errors that slip through prescribing, typing, or labeling mistakes—errors that could kill. It’s not optional. It’s not just good practice. In most states and countries, it’s the law for high-risk meds like blood thinners, insulin, and opioids.
A pharmacy double-check, a mandatory verification step where two trained professionals review a prescription before it’s dispensed. Also known as final verification, this step catches errors that slip through prescribing, typing, or labeling mistakes—errors that could kill. isn’t about distrust. It’s about human error. A doctor might write "0.5 mg" but the system reads "5 mg." A pharmacist might miss that your new blood pressure pill interacts with your old thyroid med. A tech might grab the wrong bottle because the labels look similar. One person can miss it. Two people, checking independently, almost always catch it. Studies show this step reduces dispensing errors by up to 85%. That’s not a number—it’s your life.
This isn’t just about pills. It’s about timing, too. A drug interaction, a harmful or reduced effect when two or more medications are taken together. Also known as medication clash, it can turn a safe treatment into a crisis. Like when fiber supplements block your thyroid med, or when a common painkiller spikes your potassium to dangerous levels. The second pharmacist doesn’t just verify the dose—they cross-check your full med list. They see if that new antidepressant clashes with your heart drug. They spot if your statin dose is too high for your kidney function. They know what your last refill was—and if something looks off, they stop it.
You might think, "I’ve been taking this for years, why check again?" But your body changes. Your kidneys slow down. You start a new supplement. You forget to tell your doctor about the OTC sleep aid. The double-check doesn’t assume anything. It asks: Is this right today? Not last year. Not when you were younger. Not when you didn’t have diabetes.
And it’s not just the pharmacist. You’re part of it too. If you’ve ever asked, "Wait, this pill looks different," you’ve done your part. That question saves lives. If your prescription suddenly costs way more than last time, that’s a red flag—maybe the wrong drug was filled. If the label says "take with food" but your pill is a capsule that melts in your mouth, ask. You don’t need to be a doctor to spot something wrong. You just need to pay attention.
The posts below show how this simple step connects to everything else: how fiber supplements can block meds, why statins cause muscle pain, how hyperkalemia hides in plain sight, and why timing matters more than you think. Each story is a reminder: medication safety isn’t about big breakthroughs. It’s about small checks done right, every single time. And if you’ve ever wondered why your pharmacist asks the same questions again and again—now you know. They’re not being repetitive. They’re protecting you.