Vasculitis: Understanding Autoimmune Inflammation of Blood Vessels
 Dec, 1 2025
Dec, 1 2025
When your immune system turns on your own blood vessels, things go wrong fast. Vasculitis isn’t just one disease-it’s a group of rare but serious conditions where your body’s defense system attacks the walls of your arteries and veins. This inflammation can narrow, weaken, or even block blood flow to vital organs. Left untreated, it can lead to kidney failure, stroke, heart attack, or tissue death. The good news? With early diagnosis and the right treatment, most people can regain control of their health.
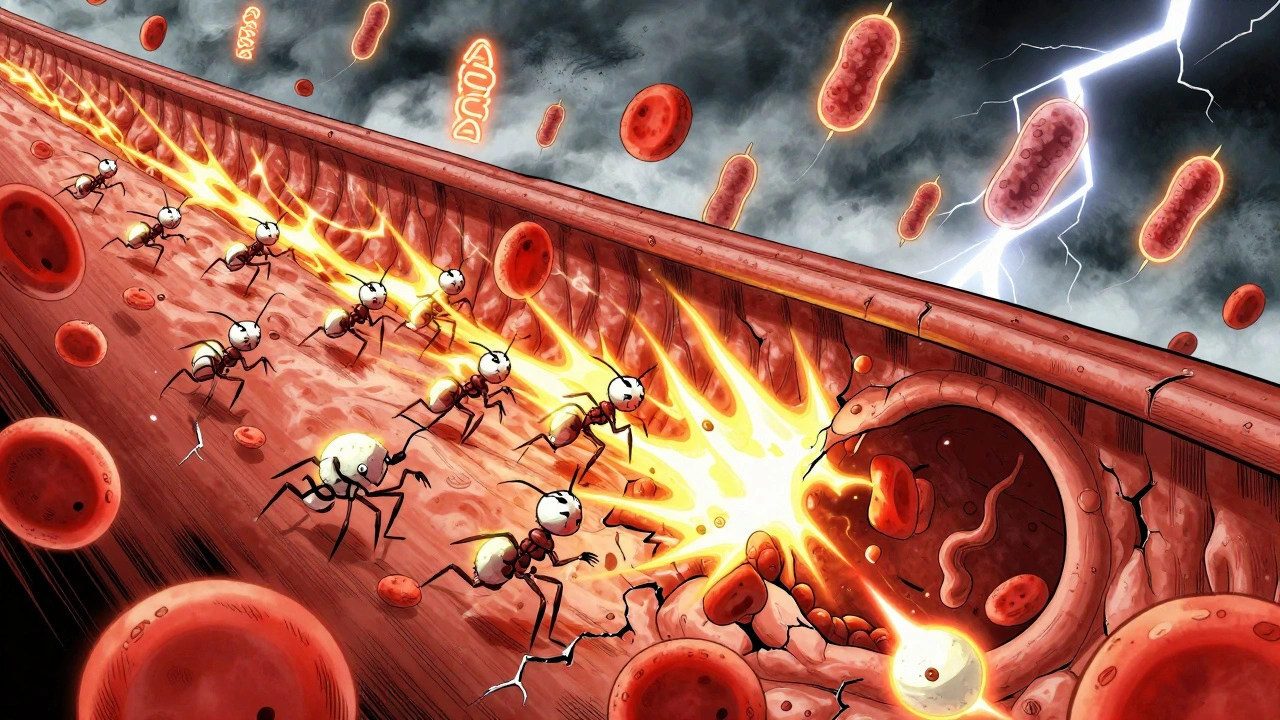
What Happens Inside Your Blood Vessels?
Your blood vessels-arteries, veins, and capillaries-are the highways of your body. They carry oxygen, nutrients, and immune cells to every organ. In vasculitis, the immune system mistakes the vessel walls for invaders. White blood cells swarm the area, causing swelling, damage, and scarring. Over time, the vessel wall thickens, the lumen narrows, or worse, an aneurysm forms. In severe cases, the vessel ruptures or clots off completely. This damage doesn’t happen evenly. Different types of vasculitis target different vessel sizes:- Large-vessel vasculitis affects the aorta and its major branches. Giant cell arteritis (GCA) is the most common, usually hitting people over 50. It often attacks the temples, causing headaches, jaw pain when chewing, and sometimes sudden vision loss.
- Medium-vessel vasculitis targets arteries like those feeding the kidneys, intestines, or skin. Polyarteritis nodosa (PAN) falls here, and Kawasaki disease-which mostly affects children under 5-can cause coronary artery aneurysms if not treated quickly.
- Small-vessel vasculitis is the most dangerous because it hits capillaries in the kidneys, lungs, and nerves. Conditions like granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA) are all ANCA-associated. That means a specific antibody, called ANCA, is often found in the blood.
Each type has its own pattern. But the result is always the same: less blood flow means less oxygen. Organs start to fail.
How Do You Know If You Have It?
Vasculitis is sneaky. Its symptoms look like the flu, arthritis, or even aging. That’s why most people wait 6 to 12 months before getting a correct diagnosis. Common signs include:- Red or purple spots, bumps, or bruises on the skin-especially on the lower legs
- Joint pain or swelling
- Constant fatigue and fever with no clear cause
- Numbness or tingling in hands or feet
- Coughing up blood or shortness of breath
- Stomach pain, nausea, or bloody stools
- Headaches, scalp tenderness, or jaw pain when eating
- Loss of appetite or unexplained weight loss
Some people feel fine until their kidneys start failing. That’s why doctors always check urine for blood or protein, even if you don’t feel sick. Blood tests often show high levels of inflammation: ESR over 50 mm/hr or CRP above 5 mg/dL. But the real clue? ANCA antibodies.
For GPA, c-ANCA targeting proteinase-3 shows up in 80-90% of cases. For MPA and EGPA, p-ANCA targeting myeloperoxidase is more common. But no single test confirms vasculitis. You need the full picture: symptoms, blood work, imaging, and often a biopsy.
How Is It Diagnosed?
There’s no single test for vasculitis. Doctors piece it together like a puzzle.- Blood tests check for inflammation markers and ANCA antibodies. But remember: ANCA can be positive in other conditions, and some people with vasculitis test negative.
- Imaging shows vessel damage. A CT or MRI can reveal inflamed arteries in the head, chest, or abdomen. An ultrasound might show thickened walls in the temporal artery for giant cell arteritis.
- Tissue biopsy is still the gold standard. A small sample from the skin, kidney, lung, or nerve can show the telltale signs: immune cells tearing through vessel walls, fibrinoid necrosis, or leukocytoclastic debris. A skin biopsy in someone with purple spots can confirm small-vessel vasculitis.
- Urine tests are non-negotiable. Even if you feel fine, protein or red blood cells in your urine mean your kidneys are under attack.
The Five Factor Score helps doctors judge how serious it is. It looks at five high-risk features: kidney involvement, heart issues, gastrointestinal bleeding, nerve damage, or lung bleeding. The more you have, the higher your risk of death without aggressive treatment.

Treatment: Stopping the Attack
Treatment depends on the type, severity, and organs involved. But the goal is always the same: shut down the immune attack and protect your organs.For severe cases, doctors start with high-dose steroids like prednisone-often 0.5 to 1 mg per kg of body weight daily. That’s a lot. But it’s necessary to calm the inflammation fast.
Then comes the immune-suppressing drug:
- Cyclophosphamide has been the go-to for decades. It’s powerful but comes with risks like bladder damage and infertility.
- Rituximab targets B-cells-the immune cells that make ANCA. It’s now preferred for many cases because it’s just as effective and safer long-term.
- Avacopan is the newest player. Approved in 2021, it blocks a protein called C5a that drives inflammation. In clinical trials, patients on avacopan plus low-dose steroids had the same remission rates as those on high-dose steroids-but with 2,000 mg less steroid exposure over a year. That means fewer side effects: less weight gain, fewer broken bones, lower diabetes risk.
Once remission is reached, maintenance therapy begins. This lasts 18 to 24 months or longer. Options include:
- Methotrexate
- Azathioprine
- Rituximab (given every 6 months)
For giant cell arteritis, steroids are still first-line. But now, tocilizumab-an IL-6 blocker-is approved to help reduce steroid doses. For Kawasaki disease, high-dose IV immunoglobulin and aspirin are standard. And for Buerger’s disease? Quitting tobacco isn’t optional. If you keep smoking, nothing else works.
What’s the Long-Term Outlook?
The good news: most people go into remission. About 80-90% of those with ANCA-associated vasculitis do. But relapse is common-nearly half within five years.Survival rates vary. For polyarteritis nodosa, someone with no major organ damage has a 95% chance of living five years. If they have two or more major organ issues? That drops to 50%. That’s why early treatment matters so much.
People with giant cell arteritis often need steroids for years. Long-term steroid use brings risks: osteoporosis, cataracts, diabetes, high blood pressure. That’s why newer drugs like tocilizumab and avacopan are game-changers-they help you get off steroids faster.
Children with Kawasaki disease need lifelong heart monitoring. About 1 in 5 untreated kids develop coronary artery aneurysms. Even with treatment, some need regular echocardiograms for years.

What’s New in Research?
Science is moving fast. Researchers are looking for better ways to predict flares before they happen. Blood tests for B-cell activating factor (BAFF) and urinary MCP-1 are showing promise as early warning signs.Clinical trials are testing new drugs:
- Mepolizumab for EGPA: Early results show it cuts relapse rates by half.
- Abatacept for giant cell arteritis: Aiming to reduce steroid dependence.
- Belimumab: Already used in lupus, now being tested for vasculitis.
The Vasculitis Clinical Research Consortium is building a national database to track outcomes and find patterns. The goal? Personalized treatment. Not one-size-fits-all, but the right drug for your type, your antibodies, your risk profile.
Living With Vasculitis
It’s not just about medicine. It’s about lifestyle, monitoring, and support.- Get vaccinated. Steroids weaken your immune system. Stay up to date on flu, pneumonia, and shingles shots.
- Protect your bones. Take calcium and vitamin D. Ask about bone density scans.
- Watch for infection. A fever that won’t go away? Call your doctor. It could be a flare-or something else.
- Stay active. Gentle exercise helps with fatigue and joint pain. Walking, swimming, yoga.
- Find your community. Support groups, online forums, patient advocacy groups-they help you feel less alone.
Vasculitis isn’t curable. But it’s manageable. Many people live full lives-work, travel, raise families. The key is staying ahead of it. Regular check-ups. Blood tests. Listening to your body.
If you’ve been told your symptoms are ‘just stress’ or ‘old age’-get a second opinion. Vasculitis is rare, but it’s real. And if you’re feeling off, don’t wait six months to find out why.
Can vasculitis go away on its own?
Some mild forms, like small skin vasculitis, can resolve without treatment. But systemic vasculitis-especially when it affects kidneys, lungs, or nerves-won’t go away on its own. Delaying treatment risks permanent organ damage. Always see a rheumatologist if symptoms persist.
Is vasculitis hereditary?
No, vasculitis isn’t directly inherited. But some genetic factors may make certain people more likely to develop it when triggered by infections, medications, or environmental factors. It’s not passed down like cystic fibrosis or sickle cell disease.
Can you get vasculitis from an infection?
Infections don’t cause vasculitis directly, but they can trigger it in people who are genetically prone. Hepatitis B and C, for example, are linked to certain types of vasculitis. After a viral illness, the immune system can go haywire and start attacking blood vessels.
Does diet affect vasculitis?
No specific diet cures vasculitis. But eating anti-inflammatory foods-like fruits, vegetables, fatty fish, nuts, and whole grains-can help manage overall inflammation. Avoid processed foods and excess sugar, which can worsen immune activity. If you’re on steroids, watch your sodium and sugar intake to protect your blood pressure and blood sugar.
Can vasculitis come back after treatment?
Yes. Relapse rates are high-up to 50% within five years for ANCA-associated vasculitis. That’s why maintenance therapy is so important. Even if you feel fine, regular blood tests and doctor visits are critical. Early detection of a flare means faster treatment and less damage.
What kind of doctor treats vasculitis?
A rheumatologist is the main specialist. They’re trained in autoimmune diseases and know how to interpret ANCA tests, biopsies, and imaging. In some cases, you’ll also work with nephrologists (kidneys), pulmonologists (lungs), or neurologists (nerves)-depending on which organs are affected.
When to Seek Help Immediately
Call your doctor or go to the ER if you have:- Sudden vision loss or double vision
- Coughing up blood
- Severe chest or abdominal pain
- Weakness or numbness on one side of the body
- Dark urine or no urine for 12+ hours
These could mean your blood vessels are blocking critical blood flow. Minutes matter.

Chris Wallace
December 2, 2025 AT 13:15Man, I never realized how sneaky this stuff is. I had a buddy who kept getting these weird purple spots on his legs for months, and everyone told him it was just allergies or stress. He finally saw a rheumatologist after collapsing from kidney pain - turned out to be GPA. They started him on rituximab and avacopan, and now he’s hiking again. It’s wild how fast things can go south if you ignore the small signs.
Also, the part about ANCA testing being unreliable? So true. My cousin tested negative for years but had all the symptoms. Biopsy was the only thing that confirmed it. Doctors need to stop treating labs like gospel.
And don’t even get me started on how long it takes to get a referral. By the time you see a specialist, half your organs are already whispering for help.
But yeah - the fact that we’ve got drugs like avacopan now that slash steroid use? That’s hope. Real, tangible hope. I’m just glad someone finally wrote this out clearly instead of burying it in medical jargon.
Also, get your shingles shot. Seriously. Steroids turn you into a walking petri dish.
Thanks for posting this. Needed this.
william tao
December 3, 2025 AT 23:08It is imperative to note, with the utmost gravity, that the medical establishment has, for decades, systematically underdiagnosed vasculitis due to a profound lack of education among primary care physicians - a failure of epic proportions. The current paradigm of diagnostic delay - six to twelve months - is not merely negligent; it is criminal. The fact that we rely on biopsy, an invasive and often inaccessible procedure, as the ‘gold standard,’ speaks volumes about the archaic nature of modern medicine. We must demand molecular diagnostics, population-wide screening protocols, and mandatory rheumatology rotations for all internists - or more lives will be needlessly lost. This is not science. This is triage roulette.
Sandi Allen
December 5, 2025 AT 12:17Wait - so you’re telling me the government and Big Pharma are letting people die from ‘rare’ diseases so they can keep selling steroids and rituximab? And now they’re pushing AVACOPAN - which is just another patent-protected drug that costs $12,000 a month - to make us think they’re ‘innovating’?!!
ANCA? That’s a lab trick. The real cause? Fluoride in the water. EMF radiation from 5G towers. And the vaccines. They’re all connected. I’ve seen the studies - they’re buried in PubMed under ‘autoimmune mimicry.’
And why do they always say ‘biopsy’? Because they don’t want you to know you can reverse this with turmeric, magnesium, and cold plunges! I’ve cured my own vasculitis - no drugs - and now I’m 72 and running marathons!
They don’t want you to know this. They want you dependent. Wake up.
Also - who funded this article? NIH? FDA? Tell me the truth.
Shubham Pandey
December 5, 2025 AT 23:18Easy to write. Hard to live. My uncle had PAN. Steroids made him gain 50 lbs, broke his hip, got diabetes. Then they gave him cyclophosphamide - he lost his hair, got bladder cancer. He’s gone now.
Avacopan sounds good. But who gets it? Not people like us. Not in India. Not even in most US hospitals.
Real talk: medicine is for the rich.
Genesis Rubi
December 7, 2025 AT 14:22Okay but like - why are we even talking about this like it’s some mysterious disease? It’s just your immune system being extra. Like, if you ate clean, stopped stress, and didn’t drink that fake coffee from Starbucks, you wouldn’t need all these drugs.
Also - who even gets this? Like, white people over 50? That’s just what happens when you stop working out and start taking pills for everything.
And why are we praising avacopan? It’s probably just a placebo with a fancy name. I bet it’s made in Switzerland and costs a fortune. We don’t need it. We need discipline.
Also - why are you letting doctors tell you what to do? You’re an American. Be strong.
Doug Hawk
December 8, 2025 AT 03:57ANCA-associated vasculitis is a fascinating paradigm of immune dysregulation - particularly the pathogenic role of neutrophil extracellular traps (NETs) in vascular injury. The shift from cyclophosphamide to rituximab reflects a broader transition from cytotoxic immunosuppression to targeted B-cell depletion - a molecular precision medicine approach.
But here’s the underdiscussed issue: the heterogeneity of ANCA specificity. c-ANCA vs p-ANCA isn’t just serological noise - it correlates with distinct endotypes. Proteinase-3 targeting drives more upper airway and pulmonary involvement, while MPO is linked to renal-predominant disease.
And avacopan? Brilliant. C5aR1 blockade interrupts the complement-amplified neutrophil activation cascade without broad immunosuppression. But long-term safety data? Still limited. We need real-world registries.
Also - biopsy remains irreplaceable. No imaging modality can replicate histologic evidence of fibrinoid necrosis.
Still - the real breakthrough is recognizing vasculitis as a spectrum, not a checklist. We’re moving toward phenotype-driven therapy. That’s the future.
John Morrow
December 9, 2025 AT 23:41Let’s be honest - this article reads like a pharmaceutical brochure dressed up as patient education. Avacopan? Rituximab? Tocilizumab? All expensive, all patented, all pushed by companies with lobbying budgets bigger than your local hospital’s entire rheumatology department.
And yet, they gloss over the fact that most patients with vasculitis are middle-aged or elderly - people who can’t afford the co-pays, who live on fixed incomes, who have to choose between rent and their maintenance meds.
They talk about ‘remission’ like it’s a victory. But what about the 40% who relapse? What about the neuropathy that never goes away? The chronic fatigue? The steroid-induced cataracts? The osteoporosis from five years of prednisone?
This isn’t medicine. It’s damage control with a side of hope porn.
And don’t get me started on ‘support groups.’ They’re just echo chambers for people too scared to admit they’re dying.
Real talk: we’re not curing vasculitis. We’re just making it a lifelong billing cycle.
Kristen Yates
December 11, 2025 AT 19:52I work in a hospital in rural Ohio. We don’t have rheumatologists on staff. We have one PA who tries to read the guidelines. I’ve seen patients come in with leg ulcers and numb hands, and the first thing they’re told is ‘it’s probably just arthritis.’
It breaks my heart. People wait so long because they don’t know what to look for. Or they don’t have the time or money to push for answers.
This post? It’s the kind of thing we should hand out in waiting rooms. Not just to patients - to nurses, EMTs, even the front desk staff. If someone walks in with unexplained fever, weight loss, and purple spots - even if they’re young - don’t dismiss it.
Knowledge saves lives. Even if it’s just one person who reads this and finally gets tested.
Thank you.
Saurabh Tiwari
December 11, 2025 AT 20:39So many people think autoimmune stuff is just ‘bad luck’… but honestly, in India, we see a lot of post-dengue or post-hepatitis cases that turn into vasculitis. The body’s defense goes rogue after fighting hard.
Also - avacopan sounds cool but we don’t even have it here. Steroids are still king. And yeah, they wreck your bones.
But I’m glad someone wrote this. My cousin had GPA. He’s doing okay now on rituximab. He says the hardest part isn’t the meds - it’s the loneliness. No one gets it unless they’ve been there.
Stay strong, everyone. 🙏
Michael Campbell
December 13, 2025 AT 00:28They’re lying about the vaccines. This is all from the shots. I know people who got vasculitis after their third dose. The CDC won’t admit it because they’re in bed with Pfizer. Same with 5G. Same with the water. You think this is coincidence? It’s a pattern.
And don’t tell me about ‘biopsies.’ They’re just covering up the truth. The real test is in your blood - if you know where to look.
Also - why do they always say ‘rare’? Because they don’t want you to know how many people are dying. They’re hiding it.
Wake up. They’re poisoning us. And you’re letting them.
Victoria Graci
December 13, 2025 AT 17:32There’s something almost poetic about the body turning against itself - a silent civil war inside the arteries. Vasculitis isn’t just disease; it’s betrayal. The immune system, our lifelong bodyguard, becomes the assassin. And we’re left wondering: was it the toxins? The stress? The grief? The unspoken trauma that settled into our cells like dust?
It’s not just about antibodies and biopsies. It’s about the weight of living in a world that tells you your pain is ‘in your head’ - until it isn’t.
And yet - we persist. We take the pills. We show up for the labs. We walk even when our feet ache. We love even when our bodies feel like strangers.
This isn’t just medicine. It’s resilience in the form of a blood test.
Thank you for writing this. It’s the kind of truth that doesn’t shout - but lingers.
Saravanan Sathyanandha
December 14, 2025 AT 00:37As someone from India who has worked with rheumatology units in both urban and rural settings, I can attest that the challenges are not just medical but systemic. Access to ANCA testing, biopsy facilities, and newer drugs like avacopan remains severely limited outside major cities. Yet, the clinical presentation is identical - the same purple skin lesions, the same kidney failure, the same silent progression.
We need training programs for primary care physicians. We need tele-rheumatology networks. We need affordable generic alternatives.
But beyond that - we need dignity. Patients deserve to be heard before they collapse. They deserve to be believed before they lose a limb or a kidney.
This article is a step. But real change requires policy, not just prose.
Thank you for highlighting the human side - not just the science.
alaa ismail
December 15, 2025 AT 22:49My mom had GCA. She was blind in one eye for three weeks before they figured it out. Steroids saved her sight but gave her diabetes. She’s 80 now. Still walks her dog every morning.
Just wanted to say - you’re not alone. And yeah, it sucks. But you’re still here. That counts.
ruiqing Jane
December 17, 2025 AT 16:22This is the kind of information that should be mandatory reading for every high school health class. Vasculitis isn’t rare - it’s ignored. And people die because we don’t teach them to listen to their bodies.
To anyone reading this who’s been told ‘it’s all in your head’ - I believe you. Keep pushing. Get the blood work. Demand the biopsy. Your life matters more than a doctor’s schedule.
You are not your symptoms. You are not your diagnosis. You are the person who fought through the fog - and kept going.
Keep going.
Chris Wallace
December 18, 2025 AT 20:19Man, I read your comment about the PA in rural Ohio - that hit me hard. My sister’s PCP dismissed her for 11 months. She finally got seen at a teaching hospital because she showed up with blood in her urine and screamed until someone listened.
That’s the real story. Not the drugs. Not the ANCA. It’s the system failing people until they’re screaming into the void.
Thanks for saying that. We need more voices like yours.