Fiber for GI Health: Soluble vs. Insoluble Choices
 Dec, 23 2025
Dec, 23 2025
Most people know fiber is good for you-but few know how it actually works in your gut. If you’ve ever felt bloated after eating salad, or struggled with constipation despite eating bran cereal, you’re not alone. The problem isn’t fiber itself. It’s not knowing which kind you need-and when.
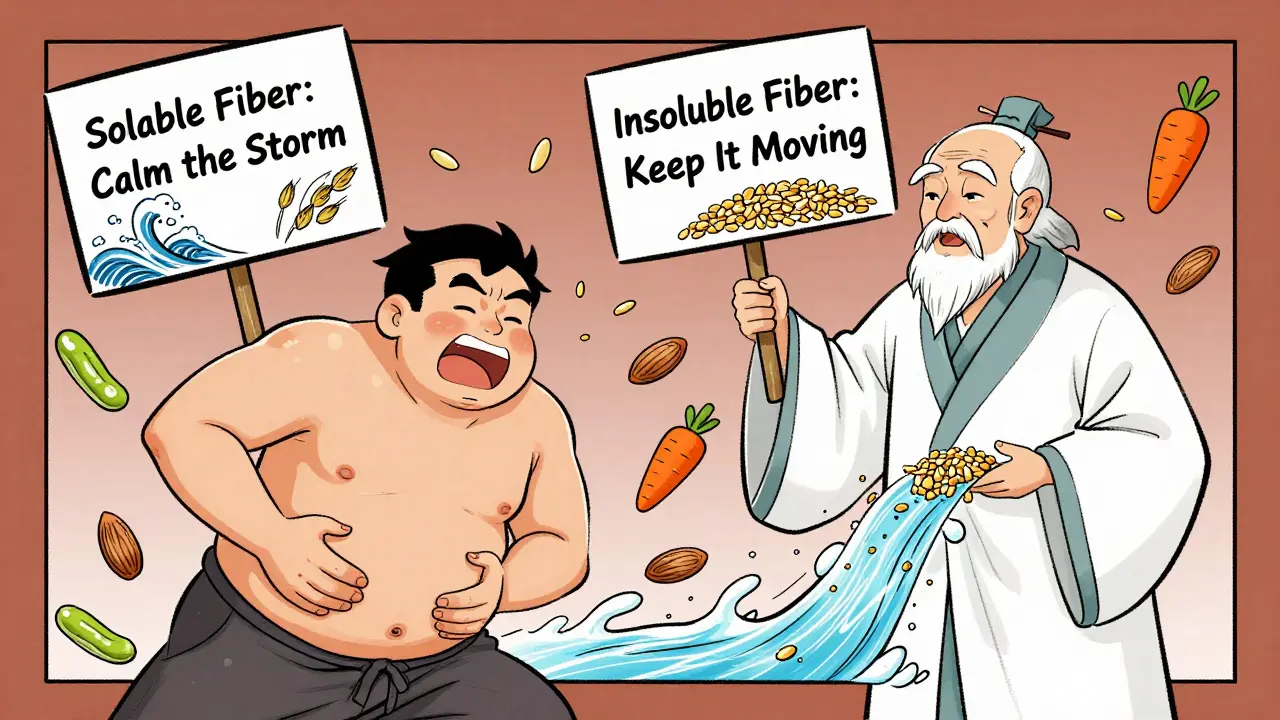
What’s the Difference Between Soluble and Insoluble Fiber?
Fiber doesn’t break down in your digestive tract. That’s the point. It moves through your system mostly unchanged, doing its job along the way. But not all fiber is the same. There are two main types: soluble and insoluble. They work differently, come from different foods, and help with different issues.Soluble fiber dissolves in water. Think of it like a sponge soaking up liquid. It turns into a thick, gel-like substance in your intestines. This gel slows down digestion, which helps control blood sugar and lowers cholesterol. It also feeds the good bacteria in your gut, which makes short-chain fatty acids that reduce inflammation and support your immune system.
Insoluble fiber doesn’t dissolve at all. It’s like roughage-stiff and sturdy. It grabs water as it moves through your system, adding bulk to your stool and helping things move faster. It’s the reason whole grains and veggie skins make you poop more regularly.
You need both. But if you’re dealing with digestive issues, one type will help more than the other.
How Soluble Fiber Helps Your Gut
Soluble fiber is the quiet hero of gut health. It’s not flashy, but it’s doing heavy lifting behind the scenes.When you eat oats, beans, apples, or chia seeds, the soluble fiber in them turns into a gel. That gel slows the absorption of sugar into your bloodstream. Studies show this can reduce post-meal blood sugar spikes by 20-30%. That’s huge for people with prediabetes or type 2 diabetes.
It also lowers LDL (bad) cholesterol by 5-10% when you eat 5-10 grams daily. That’s about a cup of cooked lentils or two tablespoons of chia seeds. The gel binds to cholesterol particles in your gut and carries them out of your body before they get absorbed.
But the real magic? Gut bacteria. Soluble fiber is fermented by your microbiome, producing short-chain fatty acids like butyrate. Butyrate is the main fuel for the cells lining your colon. When those cells are healthy, your gut barrier stays strong. That means fewer toxins leaking into your bloodstream-and less inflammation throughout your body.
People with IBS often find relief with soluble fiber. Psyllium husk, oats, and cooked carrots help regulate stool consistency. It can ease both diarrhea and constipation because the gel acts like a buffer-thickening loose stools and softening hard ones.
How Insoluble Fiber Keeps Things Moving
If soluble fiber is the gentle healer, insoluble fiber is the enforcer. It doesn’t get digested. It doesn’t turn to gel. It just pushes through.Insoluble fiber is found in whole-wheat flour, wheat bran, nuts, seeds, and the skins of fruits and vegetables. A medium apple with skin has about 1.4 grams of soluble fiber but 2.8 grams of insoluble. The skin? That’s your gut’s best friend.
This type of fiber adds 2-3 times its weight in water to your stool. That’s why eating bran cereal or brown rice can make bowel movements easier and more regular. Research shows it can reduce constipation risk by 30-50% by speeding up transit time by 24-48 hours.
It’s also linked to lower risk of diverticular disease-small pouches that form in the colon wall. Long-term studies show people who eat more insoluble fiber have a 40% lower chance of developing these pouches.
But here’s the catch: insoluble fiber can make things worse if you have active Crohn’s disease or ulcerative colitis. During flare-ups, it can irritate inflamed tissue. That’s why doctors often recommend limiting high-fiber foods like raw veggies, nuts, and whole grains during flares.

Which One Should You Eat More Of?
The answer isn’t “soluble” or “insoluble.” It’s “both.” But how much of each?The Institute of Medicine recommends 25 grams of total fiber per day for women and 38 grams for men under 50. Most Americans get only about 15 grams. That’s half the target.
Here’s the breakdown most experts agree on:
- Two-thirds of your fiber should come from insoluble sources-whole grains, vegetables, nuts, seeds.
- One-third should come from soluble sources-oats, beans, apples, chia, flax.
That’s roughly a 2:1 or 3:1 ratio. The Mediterranean Diet nails this naturally. It’s full of whole grains, legumes, fruits, veggies, and nuts-no supplements needed.
Want to test this? Try swapping out white bread for whole grain. Add a cup of lentils to your soup. Eat an apple with the skin. Snack on almonds instead of chips. That’s how you hit your numbers without thinking about it.
Common Mistakes People Make With Fiber
You can have too much of a good thing. And most people make the same three mistakes:- Going too fast. Jumping from 10 to 30 grams of fiber in a week causes bloating, gas, and cramps. Increase by 5 grams per week. Give your gut time to adjust.
- Forgetting water. Fiber needs water to work. Without enough fluids, it turns into a brick. Drink at least 1.5-2 liters of water daily for every 25 grams of fiber you eat.
- Relying on supplements. Psyllium husk or inulin powders might help short-term, but they don’t give you the vitamins, minerals, and antioxidants that come with whole foods. Studies show isolated fiber can’t replicate the benefits of eating an entire plant.
One Reddit user in r/nutrition shared that after adding soaked chia seeds to her morning yogurt, her IBS symptoms improved within two weeks. Another said switching to whole grains and eating more beans helped her constipation-but only after she started drinking a full liter of water before bed.
Fiber and Mental Health: The Gut-Brain Link
You’ve heard of the gut-brain axis. But did you know fiber plays a direct role?The short-chain fatty acids made from soluble fiber fermentation don’t just feed your colon. They signal your brain. They trigger the release of hormones like GLP-1 and peptide YY, which make you feel full and reduce cravings. Studies show this can improve satiety by 20-25%.
People who eat more fiber also report better mood and lower anxiety. One small study tracked participants who ate beans or chia seeds daily for eight weeks. Seventy-eight percent said they felt calmer and more focused. Researchers think it’s because less gut inflammation means less systemic inflammation-which affects brain function.
Companies like Viome and Zoe are now testing individual microbiomes to predict how someone responds to different fibers. In five years, your doctor might recommend a fiber plan based on your unique gut bacteria-not just your age or gender.
What to Eat: Simple Daily Plan
You don’t need a dietitian to get enough fiber. Here’s a realistic, food-first plan:- Breakfast: Oatmeal with chia seeds and an apple (8-10g fiber)
- Lunch: Lentil soup with whole-wheat bread and a side salad (12-15g)
- Snack: Carrots and hummus or a handful of almonds (5g)
- Dinner: Brown rice, roasted broccoli, and baked beans (10-12g)
That’s 35-42 grams of fiber. No supplements. No shakes. Just real food.
If you’re starting low, begin with one change: swap white rice for brown. Add one serving of beans a week. Eat fruit with the skin. Slowly build up. Your gut will thank you.
When to See a Doctor
Fiber isn’t magic. If you’re eating enough but still having issues, something else might be going on.See a doctor if:
- You have persistent bloating, pain, or diarrhea after increasing fiber
- You’re losing weight without trying
- You notice blood in your stool
- You have Crohn’s, colitis, or other diagnosed gut conditions
For IBD patients, fiber needs to be adjusted during flares. Stick to cooked, low-residue foods. Once symptoms improve, slowly reintroduce insoluble fiber under medical guidance.
Is soluble fiber better than insoluble fiber for gut health?
Neither is better-they do different jobs. Soluble fiber feeds good bacteria, lowers cholesterol, and stabilizes blood sugar. Insoluble fiber adds bulk and prevents constipation. For overall gut health, you need both. Most experts recommend a 2:1 or 3:1 ratio of insoluble to soluble fiber from whole foods.
Can fiber help with IBS?
Yes-especially soluble fiber. Foods like oats, psyllium, apples, and carrots can ease both diarrhea and constipation by regulating stool consistency. Insoluble fiber (like raw broccoli or bran) may worsen symptoms in some people with IBS. Start slow and track what works for you.
Does fiber help with weight loss?
Yes, indirectly. Soluble fiber slows digestion and triggers hormones that make you feel full longer. Studies show it can boost satiety by 20-25%. It also helps stabilize blood sugar, reducing cravings. But fiber alone won’t cause weight loss-it works best when paired with a balanced diet and regular movement.
How much water should I drink with fiber?
Drink at least 1.5 to 2 liters of water every day for every 25 grams of fiber you consume. Without enough water, fiber can cause bloating and even constipation. Start sipping water throughout the day-not just when you eat.
Are fiber supplements a good substitute for whole foods?
No. Supplements like psyllium or inulin can help short-term, but they lack the vitamins, minerals, antioxidants, and phytonutrients found in whole plant foods. Research shows the benefits of fiber are strongest when it comes from real food-like beans, oats, fruits, and vegetables. Supplements don’t replicate that synergy.
What’s Next?
Start small. Pick one meal today and add a fiber-rich food. Maybe swap white rice for brown. Add a spoon of chia to your yogurt. Eat an apple with the skin on. Track how you feel over the next week.Your gut doesn’t need a revolution. It just needs consistency. And the right kind of fiber.

Payson Mattes
December 23, 2025 AT 16:01Okay but have you heard about the glyphosate conspiracy? The FDA knows soluble fiber binds to pesticides and flushes them out-so they push insoluble fiber in public guidelines to keep us sick. That’s why your ‘whole grains’ are actually killing your microbiome. I’ve got the leaked memo. You’re welcome.
Also, chia seeds are GMO. Always buy organic or don’t bother.
Bhargav Patel
December 24, 2025 AT 11:07The distinction between soluble and insoluble fiber is not merely physiological but ontological. Soluble fiber, in its gelatinous form, mirrors the fluidity of consciousness-slowing, modulating, harmonizing. Insoluble fiber, rigid and unyielding, is the structure of the material world itself: the bones of the earth, the husk of existence. To consume both is to reconcile the yin and yang of digestion, a microcosm of cosmic balance. One must not seek dominance of one over the other, but rather, the sacred equilibrium.
Yet, modernity, in its haste, has forgotten this. We consume fiber as commodity, not as sacrament.
Steven Mayer
December 24, 2025 AT 11:56Peer-reviewed data on SCFA-mediated gut-brain signaling is still correlational. The GLP-1 hypothesis is overhyped. Most studies use murine models with non-physiological dosing. Also, the 2:1 insoluble:soluble ratio is a myth propagated by dietitians who’ve never read a microbiome metagenome. The real optimal ratio is individualized-depends on your Akkermansia load, bile acid profile, and FUT2 genotype. Stop following arbitrary guidelines. Get a Viome test or GTFO.
Sidra Khan
December 26, 2025 AT 09:12So… fiber is good? Wow. Groundbreaking. I ate a salad yesterday and didn’t die. Who knew?
Also, IBS is just ‘your mom didn’t feed you right.’
Ademola Madehin
December 27, 2025 AT 01:41Bro this whole post is wild 😭 I went from eating only white rice to chia seeds and now I’m crying every time I poop like a baby. My wife says I’m ‘too emotional’ but she don’t understand-MY GUT IS A WAR ZONE. I’m 3 weeks in and I think I’ve made peace with my colon. 🙏
suhani mathur
December 28, 2025 AT 15:20Oh sweetie, you’re so close-but you forgot to mention that soluble fiber also reduces endotoxin translocation. And that ‘2:1 ratio’? That’s just a lazy rule of thumb. The real magic is diversity-50+ plant foods a week. Not just oats and apples. Try jicama, dandelion greens, and roasted seaweed. Your microbiome will throw you a parade.
Also, stop calling it ‘roughage.’ That term died in 1998.
Diana Alime
December 29, 2025 AT 12:04ok so i tried the chia seeds like u said and now my stomach feels like a balloon that got kicked by a goat?? i drank water i swear!! why is this happening to me?? i just wanted to be healthy not become a human air pump 😭
Chris Buchanan
December 31, 2025 AT 08:37Look-this is the most practical, science-backed fiber guide I’ve seen in years. You didn’t just dump info-you gave a roadmap. Now let’s go further: if you’re starting from zero, do this tomorrow-swap one refined carb for a whole-food fiber source. One. Single. Swap.
Do it for 7 days. Then come back and tell me you didn’t feel like a new person. I’ll wait.
Lindsey Kidd
January 2, 2026 AT 04:14Yessss this!! 🌱🍎 I’ve been telling my clients for years: it’s not about fiber supplements-it’s about eating the rainbow. My 72-year-old client went from 8g to 35g in 6 weeks with just beans, berries, and broccoli. Her IBS vanished. Her skin cleared. She started gardening again. Fiber isn’t just for your gut-it’s for your whole damn life. You’re doing amazing. Keep going. 💪
Austin LeBlanc
January 2, 2026 AT 06:42Everyone’s acting like this is new info. Newsflash: your great-grandma ate more fiber than you and never heard of ‘prebiotics.’ She ate cornbread, collards, and beans. No supplements. No Viome. Just food. You’re overcomplicating this because you’ve been sold a billion-dollar lie that you need a ‘plan’ to eat vegetables.
Go eat a potato with skin. Done.
niharika hardikar
January 2, 2026 AT 20:20While the article exhibits commendable pedagogical intent, it remains fundamentally deficient in its failure to contextualize fiber consumption within the broader framework of dietary glycemic load and phytochemical synergism. The assertion that a 2:1 ratio of insoluble to soluble fiber is universally optimal is empirically unsound. Recent longitudinal data from the EPIC cohort suggest that microbial diversity, not fiber quantity, is the primary mediator of gut health outcomes. Furthermore, the omission of fermentable oligosaccharides as a distinct category constitutes a significant taxonomic oversight.
Recommendation: Consult the WHO 2023 Guidelines on Dietary Fiber and Microbiome Health.
Rachel Cericola
January 4, 2026 AT 16:59Let’s be real: most people think ‘fiber’ means bran cereal and a sad apple. This post? It’s the wake-up call the internet needed. Soluble fiber isn’t just for cholesterol-it’s your gut’s favorite snack, and those short-chain fatty acids? They’re literally turning your colon into a wellness spa.
And yes, water matters. I had a client who ate 40g of fiber a day and still got constipated because she drank 4 ounces of water. Four. Ounces. I made her carry a 32oz bottle everywhere. Two weeks later, she cried happy tears in my office because she had a ‘normal day.’
Stop thinking of fiber as a supplement. Think of it as your body’s favorite kind of love language. Feed it. Water it. Let it breathe. And for god’s sake, stop eating white bread like it’s a personality trait.
If you’re reading this and you’ve been scared of beans? Start with canned lentils. Rinse them. Put them in a salad. You got this. I believe in you. 🌱❤️