Hypertension Medication Interactions & Risks: Essential Guide
 Oct, 24 2025
Oct, 24 2025
Hypertension Medication Interaction Checker
Check for Potential Interactions
Select medications from the dropdowns below to see if interactions may occur
Managing high blood pressure isn’t just about taking a pill every day. The real challenge often hides in the mix of drugs you’re already using, over‑the‑counter painkillers, or even supplements. Below you’ll find a practical roadmap that explains why hypertension medication interactions matter, which combos to avoid, and how to keep your treatment on track.
What are antihypertensive medications?
Antihypertensive medications are a group of drugs designed to lower elevated blood pressure and reduce cardiovascular risk. They arrived on the market in waves: thiazide diuretics in the 1950s, beta‑blockers in the 1960s, calcium‑channel blockers in the 1970s, and ACE inhibitors in the 1980s. Today the main classes include:
- Diuretics (e.g., thiazides, loop diuretics)
- Beta‑blockers (e.g., propranolol, metoprolol)
- ACE inhibitors (e.g., lisinopril, enalapril)
- Angiotensin II receptor blockers - ARBs (e.g., losartan, valsartan)
- Calcium‑channel blockers (e.g., amlodipine, diltiazem)
- Alpha‑blockers (e.g., doxazosin)
Clinical trials cited in the 2025 AHA/ACC guidelines show that achieving target blood pressure can cut stroke risk by 35‑40% and myocardial‑infarction risk by about 20‑25%.
Why drug interactions are a big deal
Polypharmacy is common: roughly 40 % of adults aged 65 + on antihypertensives take five or more other medicines. Each additional agent creates a chance for an interaction that either blunts the blood‑pressure‑lowering effect or triggers a dangerous side‑effect.
Four interaction categories guide clinicians (American College of Cardiology 2023):
- Major - must be avoided.
- Moderate - requires close monitoring.
- Minor - awareness only.
- Theoretical - insufficient evidence.
Below we dive into the most clinically relevant combos.
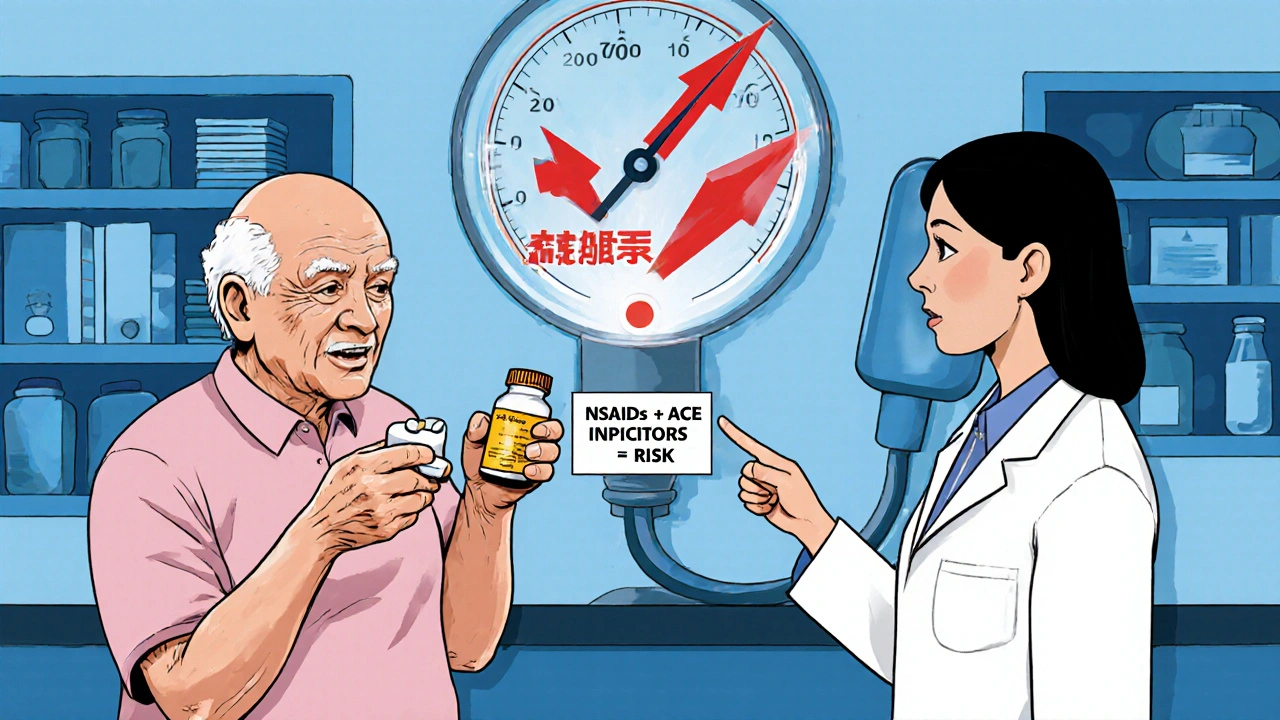
NSAIDs: The silent saboteur
Nonsteroidal anti‑inflammatory drugs (NSAIDs) are among the most frequently used over‑the‑counter meds. By inhibiting cyclooxygenase, they reduce renal prostaglandin synthesis, leading to a 15‑20 % drop in renal blood flow and a 10‑15 % dip in glomerular filtration rate. The net effect? Fluid retention and a rise in systolic blood pressure of 7‑12 mm Hg on average when paired with ACE inhibitors or ARBs.
Studies show that NSAID initiation can lift systolic pressure by 8‑10 mm Hg within 48 hours for patients already on ACE inhibitors (Weber 2022). In emergency departments, 12 % of adverse‑drug‑event visits for hypertensive patients involved an NSAID‑antihypertensive clash, most often with ibuprofen.
Safer alternatives include acetaminophen for mild pain, which demonstrates 85‑90 % efficacy without measurable blood‑pressure impact.
Beta‑blockers: Complex but powerful
Beta‑blockers such as propranolol interact with more than 200 other drugs, according to FDA labeling. Key points:
- Combined with digitalis, bradycardia risk jumps 25‑30 %.
- Co‑administration with NSAIDs dampens antihypertensive effect by 8‑12 mm Hg.
- Ethanol enhances orthostatic hypotension by 15‑20 %.
- Monoamine‑oxidase inhibitors can precipitate hypertensive crisis, increasing risk three‑ to five‑fold.
In elderly patients, beta‑blocker interactions with tricyclic antidepressants raise fall risk by 35 %.
ACE inhibitors and ARBs: Potassium and lithium pitfalls
ACE inhibitors (lisinopril) and ARBs (e.g., losartan) share a knack for raising serum potassium, especially when a patient also takes potassium supplements. Hyper‑kalemia incidence can be two‑ to three‑times higher under such combos.
Adding NSAIDs further erodes kidney perfusion, curbing the drugs’ ability to lower blood pressure by up to 12 mm Hg. Lithium toxicity climbs 30‑40 % when paired with ACE inhibitors or ARBs, demanding tighter serum level monitoring.
Calcium‑channel blockers: Statin surprises
Amlodipine and other dihydropyridine calcium‑channel blockers interact with certain statins. For instance, co‑administration with simvastatin can boost simvastatin exposure by 77 %, prompting the FDA’s 2016 limit of 10 mg daily when used with diltiazem or verapamil.
High‑dose simvastatin plus amiodarone raises rhabdomyolysis risk five‑ to seven‑fold - a severe muscle‑breakdown condition that can be life‑threatening.
Practical management: Monitoring and alternatives
Guidelines from the American Heart Association (2023) recommend the following:
- Check serum potassium every 3‑6 months for patients on ACE inhibitors/ARBs who also use NSAIDs.
- Switch chronic pain patients from NSAIDs to acetaminophen whenever possible.
- Use pharmacist‑led medication reviews - they cut hypertension‑related interaction events by 40‑45 %.
- Implement EHR alerts, which prevent 60‑65 % of dangerous NSAID‑antihypertensive combos, though alert fatigue caps real‑world adherence at about 35‑40 %.
Non‑pharmacologic tricks, such as potassium‑rich salt substitutes, can lower systolic pressure by 4‑6 mm Hg without adding interaction risk.
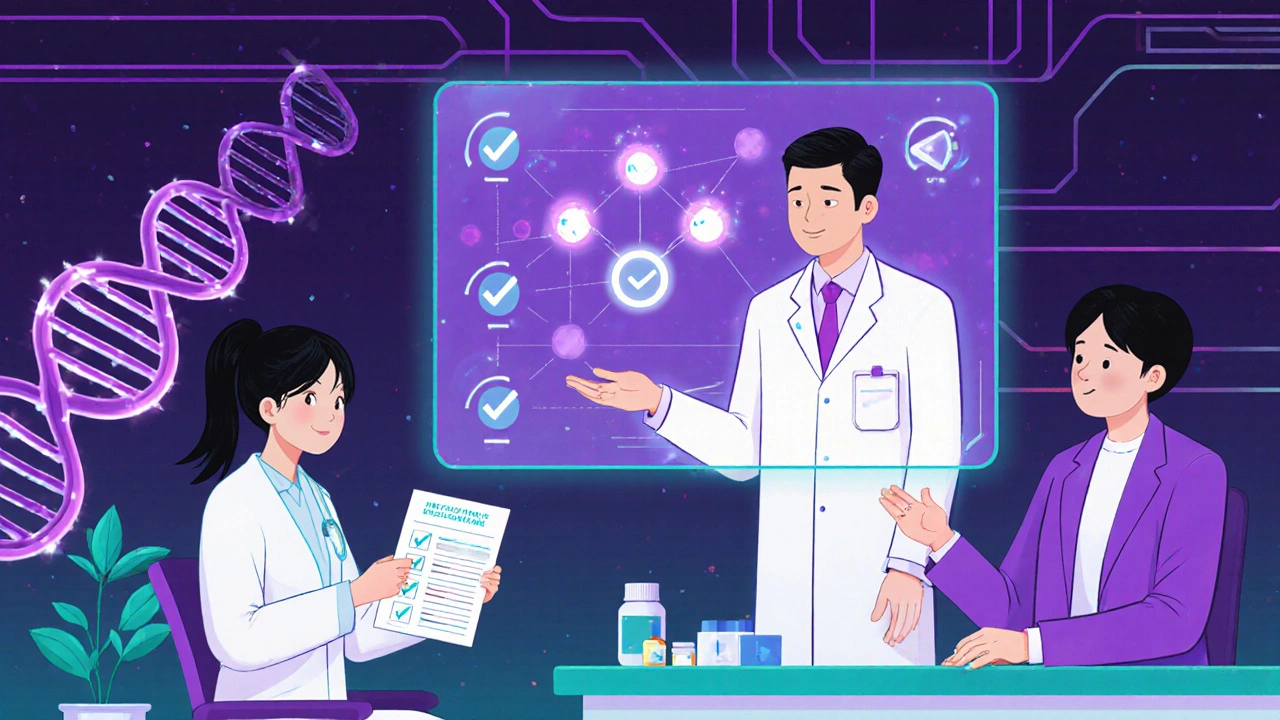
Emerging tools: Pharmacogenomics and AI
Pharmacogenomic testing is becoming mainstream. CYP2D6 poor metabolizers experience 30‑40 % higher plasma metoprolol levels when combined with fluoxetine, often requiring a 25‑30 % dose cut.
The NIH’s 2024 research identified 17 genomic markers linked to interaction susceptibility across antihypertensive classes. The FDA’s Precision Medicine Initiative now mandates that new antihypertensive labels include pharmacogenomic warnings where applicable.
Artificial‑intelligence algorithms, such as the Mayo Clinic’s 2023 model, predict significant drug‑interaction events with 88 % accuracy-far ahead of traditional decision‑support tools.
Quick checklist for clinicians and patients
- Ask every hypertensive patient about OTC NSAID and supplement use.
- Document all antihypertensive classes and dosages in a single medication list.
- When adding a new drug, cross‑check for major interactions (e.g., NSAIDs with ACE inhibitors, simvastatin with calcium‑channel blockers).
- Schedule lab monitoring (potassium, creatinine) based on the drug combo.
- Educate patients on warning signs: sudden BP spikes, muscle pain, dizziness, or palpitations.
- Consider pharmacogenomic testing for patients on beta‑blockers plus antidepressants.
Frequently Asked Questions
Can I take ibuprofen if I’m on a thiazide diuretic?
Short‑term ibuprofen can blunt the diuretic’s blood‑pressure‑lowering effect by about 5‑10 mm Hg. If pain control is essential, switch to acetaminophen or use the lowest effective ibuprofen dose for the shortest time.
What lab tests should I schedule after starting a new antihypertensive?
For ACE inhibitors or ARBs, check serum potassium and creatinine at baseline, then every 3‑6 months. Beta‑blocker patients on antidepressants may need heart‑rate monitoring and ECGs if dose changes occur.
Are potassium supplements safe with my blood‑pressure meds?
Only when a doctor approves. Combined with ACE inhibitors or ARBs, potassium can cause hyper‑kalemia, which may be life‑threatening.
How do I know if an interaction is “major” or “moderate”?
Major interactions demand avoidance (e.g., NSAIDs + ACE inhibitors). Moderate ones require close monitoring (e.g., simvastatin + diltiazem). Use reputable drug‑interaction checkers and discuss any new medication with your prescriber.
Will pharmacogenomic testing change my current hypertension regimen?
If testing reveals a CYP2D6 poor‑metabolizer status, doctors may lower beta‑blocker doses or choose drugs less reliant on that pathway, reducing the risk of side‑effects.
Bottom line
Understanding and managing hypertension medication interactions isn’t optional-it’s a core pillar of safe, effective blood‑pressure control. By staying alert to high‑risk combos, using labs wisely, and leveraging pharmacists or AI tools, both patients and clinicians can keep the numbers down and avoid costly complications.

Dahmir Dennis
November 1, 2025 AT 13:26It's baffling how many people think popping a blood‑pressure pill absolves them of any responsibility. The reality, dear readers, is that every extra over‑the‑counter tablet is a potential dagger aimed at your kidneys. If you choose ibuprofen while on an ACE inhibitor, you are essentially signing a contract with hypertension relapse. The guidelines exist for a reason, yet you treat them like optional reading material. Polypharmacy is not a badge of honor, it's a ticking time bomb wrapped in a prescription bottle. Studies cited in the 2025 AHA/ACC guidelines clearly demonstrate a 35‑40% reduction in stroke risk when interactions are avoided. Ignoring these interactions is akin to driving a sports car with the brakes disconnected. Moreover, the silent saboteur-NSAIDs-reduces renal perfusion and throws your blood pressure into the stratosphere. You might think a little naproxen is harmless, but the data shows a 7‑12 mm Hg rise in systolic pressure within 48 hours. That increase is enough to push a borderline patient into a hypertensive crisis. The same logic applies to potassium supplements paired with ACE inhibitors; hyper‑kalemia is not a myth. It's astonishing how often clinicians forget to check serum potassium every three months. The pharmacy could prevent 40‑45% of interaction events if only someone bothered to flag them. So, before you self‑medicate, remember that your autonomous choices have real, measurable consequences. In the end, the only moral high ground you can claim is by respecting the science, not by ignoring it.
Jacqueline Galvan
November 18, 2025 AT 22:06Thank you for the comprehensive overview; the evidence you presented underscores the critical nature of vigilance when prescribing antihypertensives. I would like to highlight that incorporating pharmacist‑led medication reviews has been shown to reduce adverse interaction events by up to 45 %, aligning with the guideline recommendations. Additionally, regular monitoring of serum potassium and creatinine, especially after initiating ACE inhibitors or ARBs, can preempt serious complications. Patients also benefit from education about OTC NSAID use, as early counseling often prevents unnecessary blood‑pressure spikes. Overall, a collaborative, interdisciplinary approach remains the cornerstone of safe hypertension management.
Amanda Vallery
December 6, 2025 AT 06:46Ibuprofen and thiazides are a bad combo cause they negate each other's effect.
Marilyn Pientka
December 23, 2025 AT 15:26From a pharmacodynamic standpoint the concomitant administration of non‑steroidal anti‑inflammatory agents with renin‑angiotensin system blockers precipitates a maladaptive hemodynamic shift, thereby attenuating natriuretic efficacy. Moreover, the resultant renal vasoconstriction is mediated via prostaglandin synthesis inhibition, a mechanism that warrants meticulous scrutiny in polypharmacy scenarios. In clinical lexicon this interaction is classified as 'major' and should be unequivocally avoided. The integration of decision‑support algorithms can mitigate iatrogenic risk, provided that alert fatigue is addressed through tiered notification protocols.
Jordan Levine
January 10, 2026 AT 00:06🔥💪 As proud Americans we shouldn't let foreign drug companies dictate how we manage our health! When doctors ignore the obvious dangers of NSAIDs with ACE inhibitors, they're practically handing over our nation's wellbeing to corporate greed. 😡 It's time we demand transparent labeling and empower patients to say NO to risky combos! 🇺🇸
Michelle Capes
January 27, 2026 AT 08:46Oh hey, I totally get how confusing all those meds can be 🙁. It’s really tough juggling prescriptions, especially when you’re also dealing with everyday aches. Just remember to keep a running list and maybe set a reminder for those potassium checks – it can save a lot of worry later! :)
Kathryn Rude
February 13, 2026 AT 17:26We are but vessels of fleeting blood pressure and fleeting choices the universe imposes on us yet we squabble over ibuprofen as if it were a cosmic sin 🤔 the moral of the story is simple avoid the obvious danger and let data guide you