Methotrexate vs Alternatives: Which RA Treatment Fits You?
 Oct, 5 2025
Oct, 5 2025
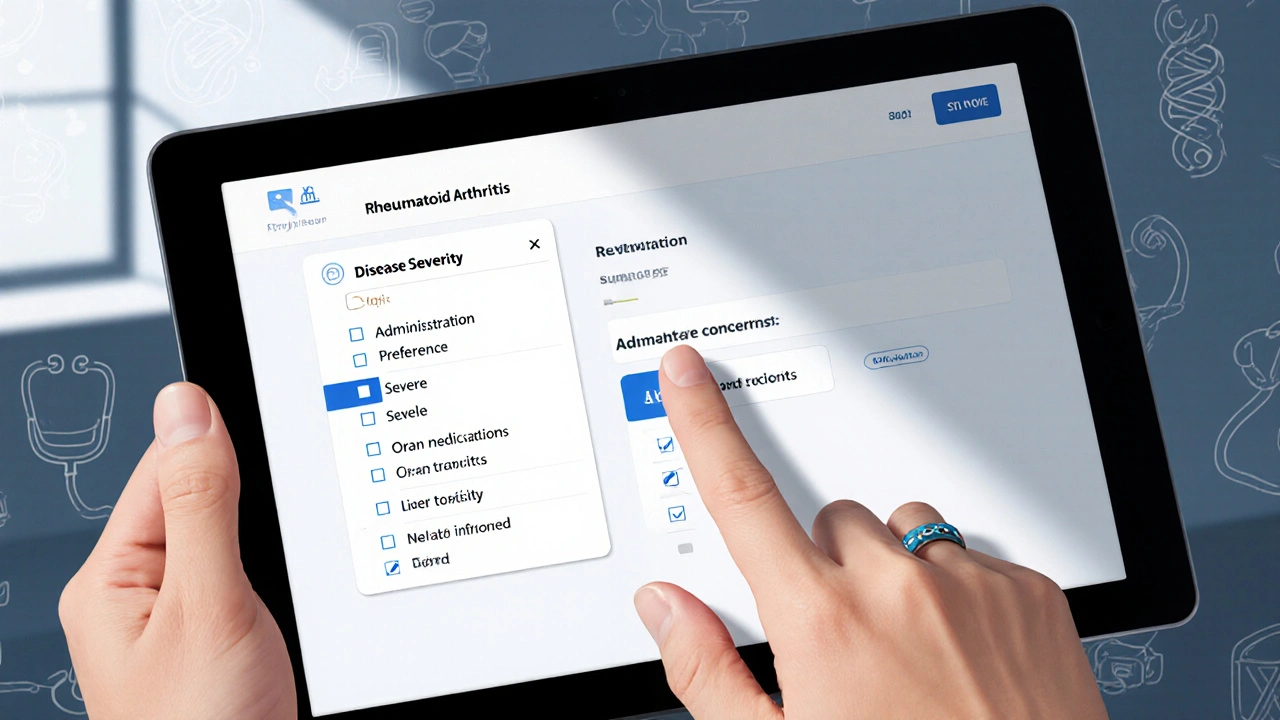
RA Drug Selector: Find Your Best Treatment Match
This interactive tool helps you explore RA treatment options by answering a few questions about your situation. It's designed to help you and your doctor discuss the best medications for your specific case.
Recommended Treatment Options
If you or someone you love has rheumatoid arthritis (RA), you’ve probably heard the name Methotrexate alternatives tossed around. Methotrexate is the go‑to drug for many, but it isn’t the only game in town. This guide walks through the most common alternatives, compares them side‑by‑side, and helps you figure out which option might suit your lifestyle and health profile.
Key Takeaways
- Methotrexate works by blocking folate metabolism; it’s effective for most patients but needs regular monitoring.
- Traditional DMARDs like Sulfasalazine and Leflunomide offer oral options with different side‑effect profiles.
- Biologic agents (e.g., Etanercept, Adalimumab) target specific inflammatory pathways and are usually reserved for moderate‑to‑severe disease.
- Hydroxychloroquine and Azathioprine are useful for milder disease or when methotrexate can’t be tolerated.
- Choosing the right drug depends on disease severity, comorbidities, cost, and how comfortable you are with injections or regular lab tests.
What Is Methotrexate?
When treating rheumatoid arthritis, Methotrexate is a folate antagonist that reduces inflammation by inhibiting the enzyme dihydrofolate reductase. It’s taken once a week, either orally or by injection, and is considered the backbone of RA therapy because it can slow joint damage in up to 70% of patients.
The drug’s strengths are its proven efficacy and relatively low cost. The downsides? Liver toxicity, mouth ulcers, and the need for blood‑test monitoring every 4‑8 weeks.
Why Look at Alternatives?
Not everyone tolerates methotrexate well. Common reasons to switch include persistent nausea, liver enzyme elevation, or a desire to avoid weekly dosing. Some patients also have contraindications-like pregnancy or significant kidney disease-that make methotrexate a risky choice. That’s where alternatives step in, offering different mechanisms, dosing schedules, or safety profiles.

Popular Alternatives Explained
Below are the most frequently prescribed drugs that can replace or complement methotrexate.
Sulfasalazine
Sulfasalazine is a sulfonamide antibiotic‑derived disease‑modifying antirheumatic drug (DMARD) that interferes with inflammatory cell signaling. It comes in tablet form, taken 2-3 times daily, and is especially handy for patients who need an oral option.
Leflunomide
Leflunomide is an oral DMARD that blocks pyrimidine synthesis, reducing the proliferation of activated T‑cells. Typical dosing starts at 20mg daily, and the drug stays in the body for weeks after stopping.
Etanercept
Etanercept is a biologic TNF‑α inhibitor administered as a subcutaneous injection twice weekly. It’s often chosen for patients with moderate to severe disease who haven’t responded to oral DMARDs.
Adalimumab
Adalimumab is another TNF‑α blocker, delivered as a self‑injectable subcutaneous dose every two weeks. It has a strong track record for reducing joint erosion.
Hydroxychloroquine
Hydroxychloroquine is an antimalarial that modulates immune activity, often used for milder RA or in combination therapy. It’s taken once daily, with a very low risk of severe side effects.
Azathioprine
Azathioprine is an immunosuppressant that interferes with DNA synthesis in rapidly dividing cells, including immune cells. It’s generally reserved for patients who can’t tolerate methotrexate or biologics.
Mycophenolate Mofetil
Mycophenolate Mofetil is an oral immunosuppressant that inhibits inosine monophosphate dehydrogenase, curbing lymphocyte proliferation. Though off‑label for RA, it’s sometimes used in refractory cases.
Side‑by‑Side Comparison
| Drug | Mechanism of Action | Typical Indications | Route & Frequency | Major Side Effects | Monitoring Needs |
|---|---|---|---|---|---|
| Methotrexate | Folate antagonist (DHFR inhibition) | RA, PsA, psoriasis | Oral/IM, once weekly | Liver toxicity, nausea, stomatitis | Liver enzymes, CBC, renal function every 4‑8weeks |
| Sulfasalazine | Anti‑inflammatory sulfonamide | RA, ulcerative colitis | Oral, 2-3× daily | Photosensitivity, GI upset, rare hepatotoxicity | Liver enzymes, CBC every 2-3months |
| Leflunomide | Pyrimidine synthesis inhibitor | RA, PsA | Oral, daily | Hypertension, liver toxicity, alopecia | Liver enzymes, CBC, BP monthly initially |
| Etanercept | TNF‑α receptor fusion protein | RA, PsA, ankylosing spondylitis | SC injection, twice weekly | Injection site reactions, infection risk | TB screen, CBC, liver enzymes every 3‑6months |
| Adalimumab | Monoclonal anti‑TNF‑α antibody | RA, Crohn’s, psoriasis | SC injection, every 2 weeks | Serious infections, malignancy risk | TB screen, CBC, liver enzymes semi‑annual |
| Hydroxychloroquine | Antimalarial immunomodulator | Mild RA, lupus | Oral, once daily | Retinal toxicity (rare), GI upset | Baseline eye exam, then annually |
| Azathioprine | Purine synthesis inhibitor | RA (when other DMARDs fail) | Oral, daily | Bone marrow suppression, liver toxicity | CBC, liver enzymes weekly → monthly |
| Mycophenolate Mofetil | Inosine monophosphate dehydrogenase inhibitor | Refractory RA, lupus nephritis | Oral, twice daily | GI upset, leukopenia | CBC, renal function every 2‑4weeks |
How to Choose the Right Option
Think of picking a drug like matching shoes to an outfit-you want comfort, style, and fit. Here are the main decision criteria you should weigh:
- Severity of disease: Mild to moderate RA often responds to oral DMARDs (methotrexate, sulfasalazine, leflunomide). Severe or rapidly progressing disease usually needs a biologic.
- Route of administration: If you dread needles, stick with oral agents. If weekly pills cause stomach upset, a subcutaneous injection might be easier.
- Side‑effect tolerance: Liver‑sensitive patients should avoid methotrexate or leflunomide. Those with a history of infections need to be cautious with biologics.
- Pregnancy plans: Hydroxychloroquine and sulfasalazine are generally safer; methotrexate is contraindicated.
- Cost & insurance coverage: Oral DMARDs are usually cheaper. Biologics can be pricey, though many plans now cover biosimilars.
- Monitoring willingness: Methotrexate, leflunomide, and azathioprine require frequent labs. Biologics need periodic infection screening but fewer routine blood draws.
Discuss these points with your rheumatologist. A shared‑decision approach leads to better adherence and outcomes.
Safety Tips & Monitoring Basics
Regardless of the drug you end up on, a few universal safety habits help keep you on track:
- Keep a medication diary-note dosages, side effects, and any missed labs.
- Never stop or change a dose without consulting your doctor; abrupt withdrawal can cause flare‑ups.
- Stay up‑to‑date on vaccinations, especially before starting biologics.
- Maintain a healthy lifestyle: balanced diet, regular exercise, and limiting alcohol (especially with methotrexate).
Frequently Asked Questions
Can I take methotrexate and a biologic together?
Yes, many rheumatologists combine methotrexate with a biologic (like etanercept) to boost effectiveness and reduce anti‑drug antibodies. This combo still requires regular liver and blood monitoring.
What’s the biggest advantage of sulfasalazine over methotrexate?
Sulfasalazine is easier on the liver and can be taken multiple times a day, making it a good fallback for patients with liver enzyme spikes on methotrexate.
Are biologics safe for older adults?
Biologics can be safe for seniors, but infection risk rises with age. Screening for latent TB and regular infection checks become especially important.
How long does it take for methotrexate to work?
Most patients notice improvement in joint pain and swelling after 6-8 weeks, but full disease‑modifying effects can take 3-6 months.
Can I become pregnant while on hydroxychloroquine?
Hydroxychloroquine is considered low‑risk during pregnancy and is often continued in women with RA or lupus who plan to conceive.
Bottom line: methotrexate remains a cornerstone of RA treatment, but a host of alternatives gives you flexibility when side effects, lifestyle, or disease severity demand a change. By weighing efficacy, safety, cost, and personal preferences, you and your doctor can craft a regimen that keeps joints moving and life enjoyable.

Mike Rylance
October 5, 2025 AT 01:53Regular monitoring of liver function tests is essential when you are on methotrexate; the schedule typically includes checks every four to eight weeks. Maintaining a consistent dosing routine helps minimize nausea and improves drug efficacy. If you notice any unusual symptoms, contact your rheumatologist promptly. Staying organized with a medication diary can also support adherence and safety.
Becky B
October 5, 2025 AT 03:33It is wise to stay aware of how pharmaceutical companies market certain RA treatments, as profit motives can sometimes shape prescribing trends. While methotrexate remains a cost‑effective first‑line option, newer biologics often carry higher price tags that may not reflect proportional benefit for every patient. Being informed about potential hidden incentives empowers you to have a more balanced discussion with your doctor. Remember that transparent communication is the foundation of good care.
Aman Vaid
October 5, 2025 AT 05:13Sulfasalazine is administered orally, usually in divided doses two to three times daily, and its absorption can be enhanced when taken with food. The drug’s mechanism involves modulation of inflammatory cell signaling, which contributes to symptom relief in mild to moderate rheumatoid arthritis. Routine laboratory monitoring focuses on liver enzymes and complete blood count every two to three months to detect early toxicity. Patients should also be cautious about photosensitivity and use adequate sun protection during therapy.
xie teresa
October 5, 2025 AT 06:53I understand how overwhelming medication choices can feel, especially when side‑effects loom large. If liver health is a concern for you, a switch to sulfasalazine or hydroxychloroquine might provide a gentler profile while still managing inflammation. Keeping a simple log of how you feel each week can reveal patterns that guide your clinician toward the best option. You deserve a treatment plan that respects both your health goals and your daily life.
Srinivasa Kadiyala
October 5, 2025 AT 08:33Sulfasalazine; oral; 2‑3× daily; watch for photosensitivity; monitor liver enzymes.
Alex LaMere
October 5, 2025 AT 10:13Try a weekly folate supplement; it can reduce methotrexate nausea 👍
Dominic Ferraro
October 5, 2025 AT 11:53Choosing the right rheumatoid arthritis medication is like assembling a puzzle where every piece matters. You start with disease severity because mild cases often respond well to oral DMARDs. Methotrexate remains the gold standard for many because of its proven track record and affordability. However, if you experience liver irritation or persistent nausea, alternatives such as sulfasalazine or leflunomide deserve a look. Sulfasalazine offers an oral route with a gentler liver impact but requires attention to photosensitivity. Leflunomide provides once‑daily dosing yet carries a risk of hypertension and liver changes. For patients whose disease progresses despite oral therapy, biologics like etanercept and adalimumab bring powerful inflammation control. These biologics are injected subcutaneously and can halt joint damage quickly, though they raise infection concerns. If you are planning a pregnancy, hydroxychloroquine stands out as a safer option compared to methotrexate. Azathioprine serves as a fallback when other DMARDs fail, but it demands close blood count monitoring. Mycophenolate mofetil is an off‑label choice for refractory cases and works by limiting lymphocyte proliferation. Cost and insurance coverage also play a pivotal role; oral drugs are generally cheaper than biologics. Talk openly with your rheumatologist about lifestyle preferences such as needle aversion or dosing frequency. Regular lab work, including liver enzymes, CBC, and kidney function, keeps you safe on most of these agents. Lastly, remember that lifestyle measures like balanced diet, moderate exercise, and limiting alcohol enhance medication effectiveness. By weighing these factors together you can craft a personalized regimen that keeps you active and pain‑free.
Jessica Homet
October 5, 2025 AT 13:33Honestly the side‑effect list for methotrexate reads like a red flag parade and most patients could do better with a milder DMARD.
Bianca Fernández Rodríguez
October 5, 2025 AT 15:13i think its important to note that many ppl dont realize the photosensitivity risk with sulfasalazine and they often forget to wear sunscreen which can lead to nasty rashs.
Patrick Culliton
October 5, 2025 AT 16:53While everyone praises biologics as miracle drugs, the long‑term infection risk often outweighs the short‑term joint benefit for many patients.
Andrea Smith
October 5, 2025 AT 18:33In the context of rheumatoid arthritis management, it is incumbent upon the treating physician to balance therapeutic efficacy with the patient’s comorbid conditions, thereby ensuring an individualized treatment paradigm.
Gary O'Connor
October 5, 2025 AT 20:13yeah, i guess if u cant take methotrexate cuz of liver probs, sulfasalazine or even hydroxychloroquine can be decent backups.
Justin Stanus
October 5, 2025 AT 21:53When evaluating treatment options, consider both the pharmacologic profile and the monitoring burden; methotrexate requires regular liver panels while drugs like leflunomide demand blood pressure checks; aligning these requirements with your lifestyle can prevent unnecessary stress.
Claire Mahony
October 5, 2025 AT 23:33Overall, the evidence suggests that starting with methotrexate is reasonable, but clinicians should not hesitate to pivot to alternatives when tolerability becomes an issue.