Advanced RCC – What You Need to Know
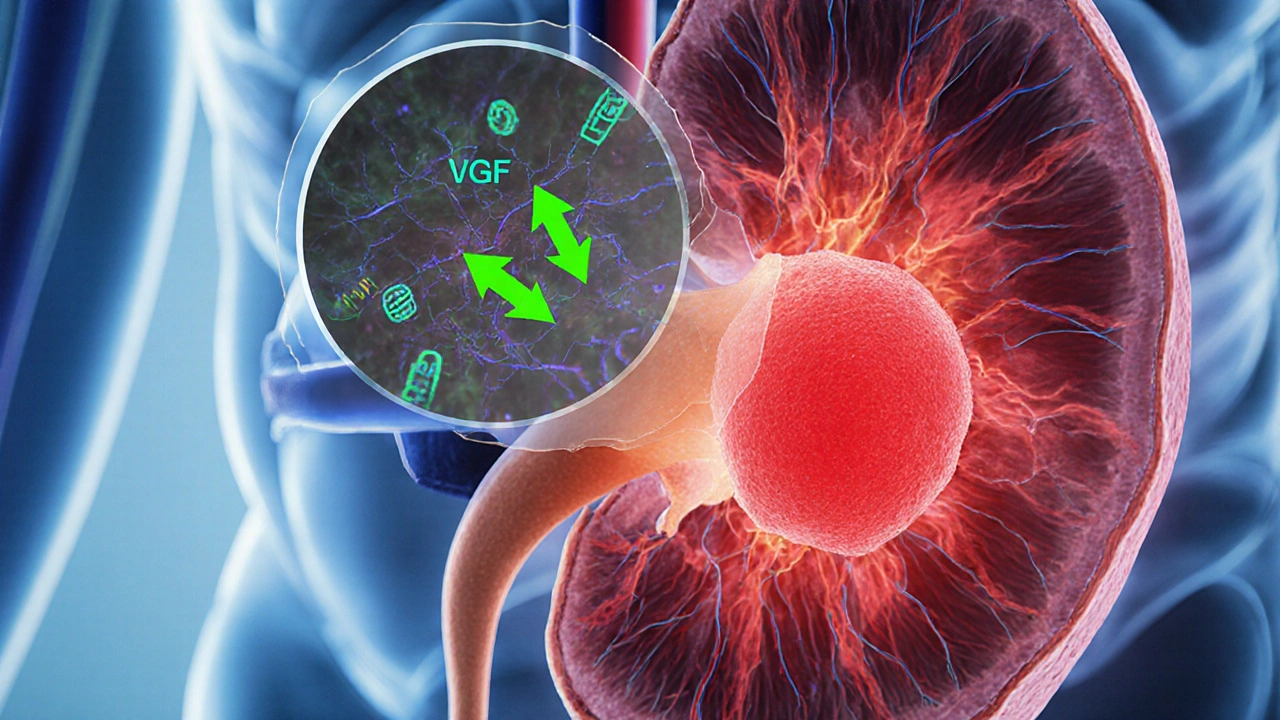
When dealing with advanced RCC, the term refers to renal cell carcinoma that has spread beyond the kidney or cannot be removed surgically. Also known as metastatic renal cell carcinoma, it demands a blend of systemic therapies rather than just surgery. Another critical piece of the puzzle is targeted therapy, drugs that block specific molecules driving tumor growth, such as VEGF or mTOR pathways. Complementing this approach, immunotherapy, treatments that unleash the body’s own immune cells to attack cancer has reshaped survival expectations. Together, these entities form the core of modern care for advanced RCC, and they set the stage for ongoing clinical trials that test new combinations and dosing strategies.
Key Treatment Options and How They Work
In practice, managing advanced RCC means selecting agents that hit the tumor from multiple angles. Targeted therapy includes drugs like sunitinib, pazopanib, and cabozantinib, which inhibit VEGF receptors and slow new blood‑vessel formation. Patients often notice side effects such as fatigue, hypertension, or hand‑foot syndrome, so dose adjustments become a routine part of care. Immunotherapy, on the other hand, relies on checkpoint inhibitors such as nivolumab or pembrolizumab to block PD‑1/PD‑L1 interactions, allowing T‑cells to recognize and destroy cancer cells. Combining a VEGF inhibitor with a PD‑1 blocker has become a standard first‑line regimen because the duo improves progression‑free survival more than either alone. Beyond these, newer agents like lenvatinib (a multi‑kinase inhibitor) paired with everolimus (an mTOR inhibitor) illustrate how blending mechanisms can overcome resistance. Real‑world data shows that patients who switch from one targeted agent to another after progression can still gain months of disease control. Meanwhile, the rise of adjuvant therapy—treatments given after nephrectomy to prevent recurrence—highlights how the line between early‑stage and advanced disease is blurring; trials now test whether early immunotherapy can keep microscopic disease at bay. Choosing the right regimen involves assessing disease burden, patient comorbidities, and personal preferences. For example, a patient with pre‑existing heart disease might avoid a VEGF inhibitor prone to raising blood pressure, while another who fears immune‑related colitis might start with a targeted agent first. Shared decision‑making, guided by up‑to‑date guidelines, ensures the plan aligns with both clinical evidence and quality‑of‑life goals.
Clinical trials remain the engine of progress in advanced RCC. They explore novel combos—like adding a CTLA‑4 inhibitor to a PD‑1 blocker—or test next‑generation kinase inhibitors that hit previously untargeted pathways. Enrollment criteria have broadened, meaning more patients with various performance statuses can access cutting‑edge therapies that may extend survival beyond what standard options offer. Keeping an eye on trial registries and discussing eligibility with oncology teams is a practical step for anyone navigating this disease. In short, advanced RCC is no longer a death sentence; it’s a complex condition that responds to a toolbox of targeted and immune‑based treatments, often refined through trial participation. Below you’ll find articles that break down specific drugs, compare treatment strategies, and give you a realistic look at what to expect when you or a loved one faces this diagnosis.