Antifungal Treatments: What Works, What to Avoid, and How to Use Them Right
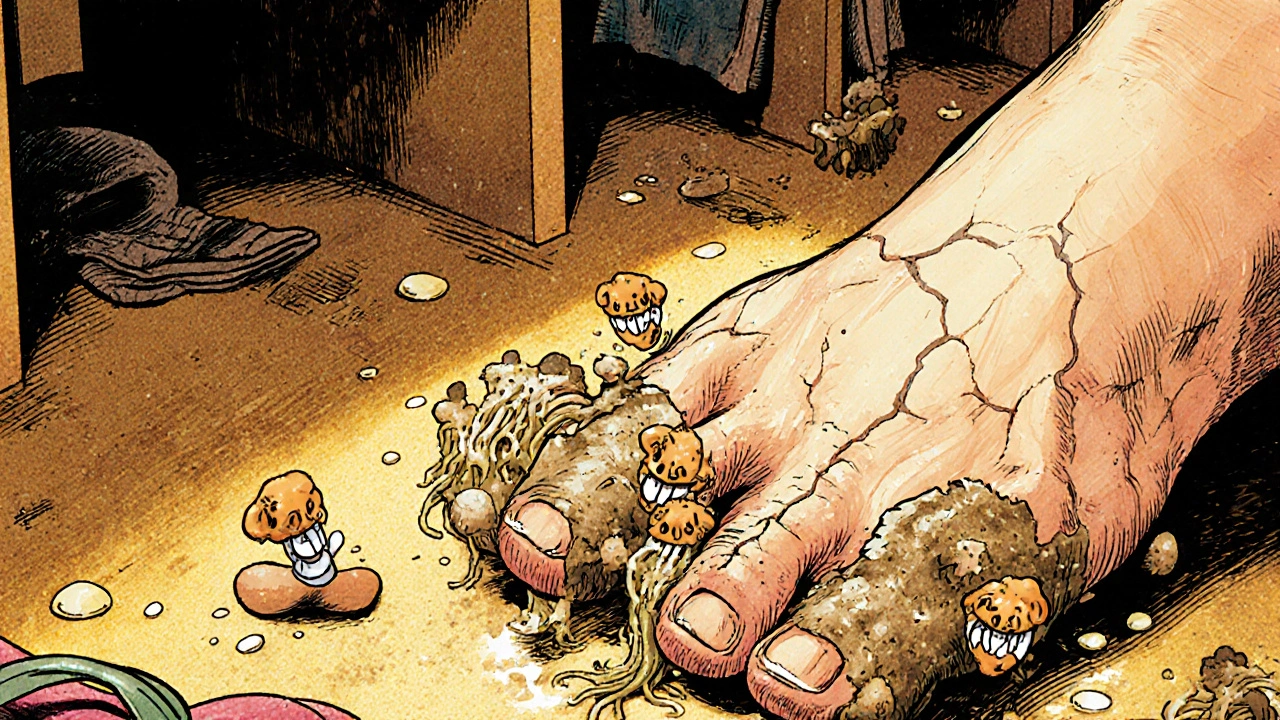
When you’re dealing with a stubborn antifungal treatment, a medication or remedy designed to kill or slow down harmful fungi in the body. Also known as antimycotic therapy, it’s not just about creams for athlete’s foot—it’s about stopping infections that can spread to nails, lungs, or even your bloodstream if left unchecked. Fungal infections are more common than most people think. Athlete’s foot, yeast infections, ringworm, nail fungus—these aren’t just minor annoyances. They can linger for months, come back after treatment, and sometimes signal something deeper, like a weakened immune system or uncontrolled diabetes.
Not all antifungal medications, drugs that target fungi without harming human cells. Common types include azoles, echinocandins, and polyenes, each with different uses and side effects. work the same way. Some are applied topically, like clotrimazole for a rash. Others, like fluconazole or itraconazole, are taken by mouth to treat internal infections. Then there are stronger IV options for serious cases, like candidemia or aspergillosis. The key isn’t just picking the strongest drug—it’s matching the right treatment to the right infection, the right location, and the right person. Using the wrong one, or stopping too early, can make the fungus resistant. That’s why so many people end up with recurring infections.
Many people try home remedies first—tea tree oil, coconut oil, vinegar soaks. Some help a little, but they won’t fix a deep nail infection or a systemic yeast overgrowth. And mixing them with prescription meds can cause reactions. Even over-the-counter antifungal creams can cause irritation if used too long or on broken skin. The real challenge? Knowing when to treat yourself and when to see a doctor. If a rash doesn’t improve in two weeks, if your nails are thickening or crumbling, or if you have fever and chills along with a fungal symptom, that’s not just a fungus—it’s a signal your body needs stronger help.
Antifungal treatments aren’t one-size-fits-all. What works for a vaginal yeast infection won’t help a scalp fungus. What’s safe for a healthy adult might be risky for someone on chemotherapy or with liver disease. That’s why the best advice isn’t just about which drug to take—it’s about understanding your body, your infection, and how to use the treatment correctly. You’ll find real-world guidance here: how to avoid common mistakes, what side effects to watch for, how long treatment really takes, and how to prevent reinfection. No fluff. No hype. Just what you need to know to get rid of the fungus—and keep it from coming back.