Calcium Channel Blockers: Uses, Types, and What You Need to Know
When working with calcium channel blockers, drugs that stop calcium from entering heart and vascular muscle cells through L‑type calcium channels. Also known as CCBs, they are a cornerstone for managing hypertension, high blood pressure that strains the heart and arteries, relieving angina, chest pain caused by reduced blood flow to the heart muscle, and controlling certain arrhythmias, irregular heartbeats that can lead to dizziness or fainting. In short, calcium channel blockers bridge the gap between blood‑vessel relaxation and heart‑rate modulation.
How They Work and Why They Matter
The key player is the L‑type calcium channel, a protein pore that lets calcium ions enter smooth‑muscle and cardiac cells. By blocking this pore, CCBs reduce the amount of calcium that triggers muscle contraction. Less calcium means blood vessels stay dilated, pressure drops, and the heart doesn’t have to pump as hard. This mechanism also slows electrical conduction through the AV node, which is why drugs like verapamil are useful for certain rhythm disorders. The result is a triple benefit: lower blood pressure, less chest‑pain episodes, and steadier heartbeats.
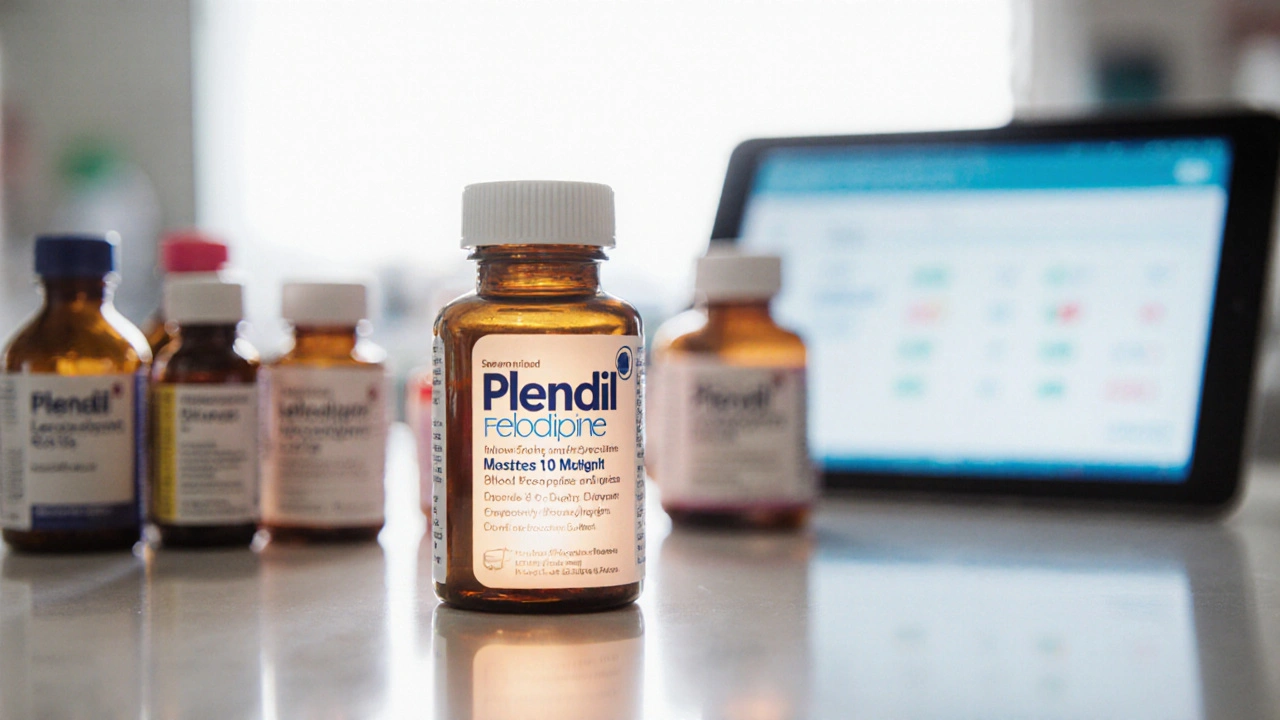
Two main families dominate the market. Dihydropyridines—such as amlodipine, nifedipine, and felodipine—preferentially relax peripheral arteries, making them ideal for pure hypertension or peripheral vascular disease. Non‑dihydropyridines—including verapamil and diltiazem—have a stronger effect on the heart’s conduction system, so they’re chosen when you need both blood‑pressure control and rhythm regulation. Knowing the difference helps clinicians match the right drug to a patient’s primary problem.
Side‑effects are generally mild but worth watching. Common complaints include swelling of the ankles, flushing, and a gentle headache as vessels widen. Non‑dihydropyridines can cause constipation or slowed heart rate, so patients on verapamil often need dose adjustments if they’re also taking beta‑blockers. Because CCBs are metabolized by the liver, drugs that inhibit CYP3A4—like certain antifungals or grapefruit juice—can raise blood levels and increase risk of toxicity. In practice, many doctors compare CCBs with ACE inhibitors, another class that lowers blood pressure by blocking angiotensin‑converting enzyme. ACE inhibitors tend to work better for kidney protection, while CCBs excel when you need strong arterial dilation.
Patient factors shape the final choice. Those with chronic kidney disease often start with a low‑dose dihydropyridine because it’s cleared mainly by the liver. Elderly patients may favor a once‑daily amlodipine to avoid frequent dosing and reduce the chance of sudden drops in blood pressure. People with a history of heart block should steer clear of non‑dihydropyridines unless a cardiologist supervises therapy. Lifestyle considerations—like a diet high in grapefruit or the use of over‑the‑counter antihistamines—also play a part in selecting the safest regimen.
Below you’ll find a curated set of articles that dive deeper into each of these angles. Whether you’re curious about the newest 2025 guidelines, looking for a side‑by‑side drug comparison, or need a step‑by‑step guide for buying a specific medication online, the collection covers practical advice, safety tips, and real‑world scenarios. Keep reading to get the details you need to make informed decisions about calcium channel blocker therapy.