Kidney-Friendly Protein: What Works, What to Avoid, and How to Eat Smart
When your kidneys aren’t working right, not all protein is created equal. kidney-friendly protein, protein sources that support kidney function without overloading it with waste products like phosphorus and nitrogen. Also known as renal-appropriate protein, it’s not about cutting protein entirely—it’s about choosing the right kind and the right amount to keep your body strong without forcing your kidneys to work overtime. Many people with chronic kidney disease (CKD) are told to reduce protein, but that can lead to muscle loss, weakness, and worse outcomes. The real goal? Balance. You need enough to maintain muscle and heal tissue, but not so much that your kidneys struggle to filter the leftovers.
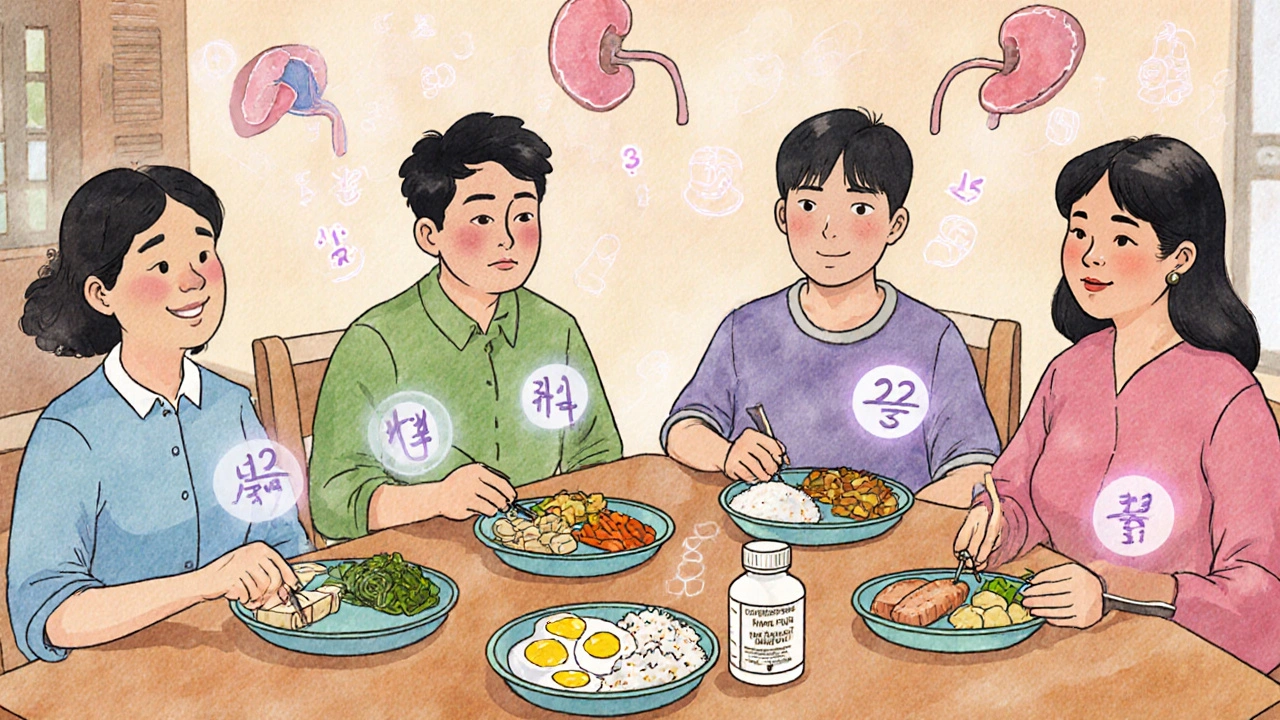
Not all protein sources are equal when it comes to kidney health. high-quality protein, proteins that contain all essential amino acids and produce less waste. Also known as complete protein, it includes eggs, lean poultry, fish, and small portions of dairy. These are easier for your kidneys to handle because they’re more efficiently used by your body. On the flip side, red meat, processed meats, and plant proteins like beans and lentils pack in more phosphorus and potassium—two minerals that can build up dangerously when kidneys fail. Even plant-based diets, often seen as healthy, can be tricky. Tofu and tempeh might seem like good swaps, but they’re high in phosphorus unless specially processed. That’s why many nephrologists recommend egg whites over whole eggs, and skinless chicken over beef.
It’s not just about what you eat—it’s about how much and how often. Most people with moderate CKD need around 0.6 to 0.8 grams of protein per kilogram of body weight daily. For a 70kg person, that’s about 42 to 56 grams total. Spread that across meals, not dumped in one big serving. Pair your protein with low-potassium veggies like cabbage or cauliflower, and avoid salt substitutes that hide potassium. And yes, protein powders? Most are loaded with phosphorus additives and should be avoided unless prescribed by a dietitian. The low-phosphorus protein, protein sources and meal plans designed to limit phosphorus intake while maintaining nutrition. Also known as renal diet protein, it’s the foundation of long-term kidney care. You don’t need fancy supplements. Real food, carefully chosen, works better.
What you’ll find in the posts below isn’t theory—it’s real-world advice from people managing kidney disease, caregivers helping loved ones, and clinicians who’ve seen what works. You’ll see how to build meals around egg whites and fish, how to read labels for hidden phosphorus, and why some "healthy" foods like nuts and dark leafy greens can backfire. There’s no one-size-fits-all, but there are clear, practical steps you can take today to eat smarter, feel stronger, and protect your kidneys longer.