Myositis: Causes, Symptoms, and Treatment Options
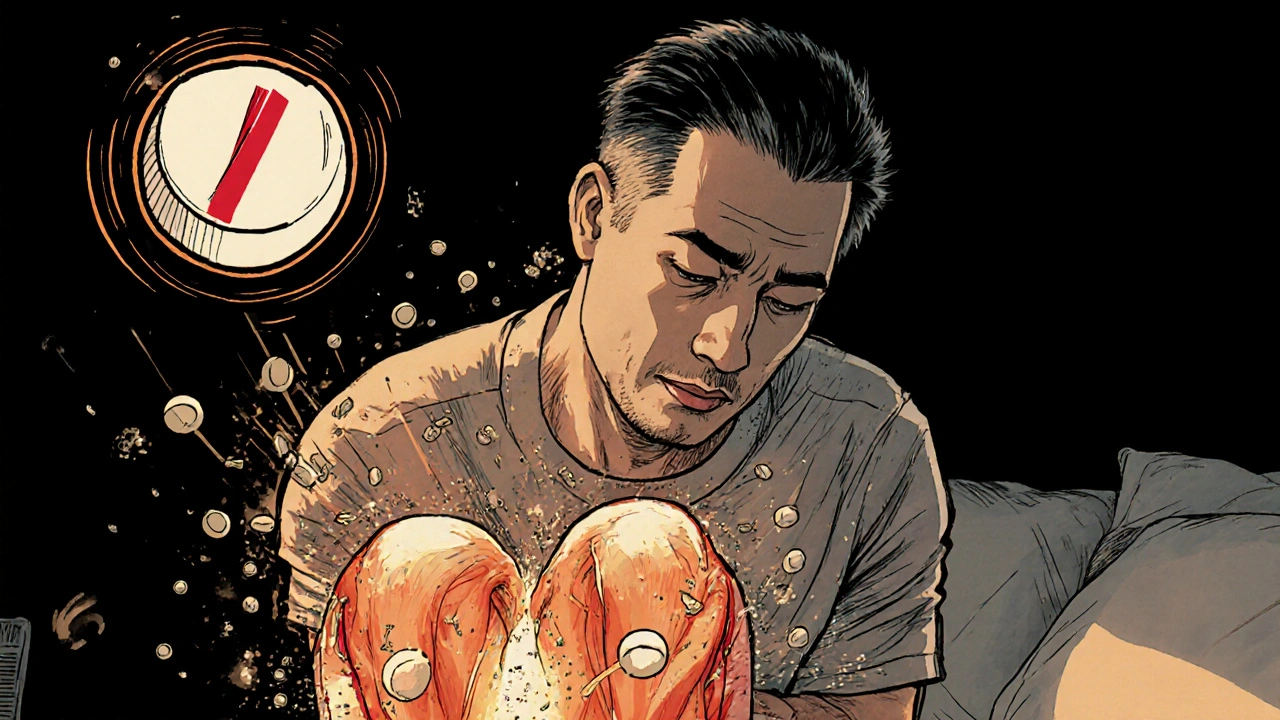
When your muscles hurt, swell, or suddenly feel weak for no clear reason, it might be myositis, an inflammatory condition that attacks muscle tissue. Also known as inflammatory myopathy, it’s not just soreness from a workout—it’s your immune system turning on your own muscles. This isn’t rare. Thousands of people live with it, often misdiagnosed as fibromyalgia or just "getting older." But myositis is real, measurable, and treatable—if you know what to look for.
There are different types, each with its own pattern. polymyositis, affects muscles symmetrically, usually in the shoulders and thighs, making it hard to stand up from a chair or lift your arms. dermatomyositis, adds a telltale rash—purple eyelids, red knuckles, or a scaly patch on the chest. Then there’s inclusion body myositis, which hits older adults and doesn’t respond well to standard treatments. It’s slow, progressive, and often mistaken for normal aging. All of them share the same core problem: muscle inflammation that steals strength.
What causes it? No one knows for sure, but it’s tied to autoimmune disorders. People with myositis often have other conditions like lupus or rheumatoid arthritis. Some cases flare after infections or even certain medications. And while it’s not contagious or genetic in the usual sense, your genes might make you more vulnerable if something triggers it.
Treatment isn’t one-size-fits-all. Steroids like prednisone are the first line—they calm the immune system fast, but long-term use brings weight gain, bone loss, and high blood sugar. That’s why doctors often add immunosuppressants like methotrexate or azathioprine to reduce steroid doses. Newer biologics are showing promise too, especially for those who don’t respond to older drugs. But medication alone isn’t enough. Physical therapy keeps muscles from shrinking. Gentle movement helps more than rest. And avoiding sun exposure? Critical if you have dermatomyositis—the rash can worsen and trigger deeper inflammation.
What you won’t find in most guides is how daily life changes. Carrying groceries, climbing stairs, even brushing your hair can become tasks that drain you. Fatigue isn’t just tiredness—it’s a deep, bone-weary exhaustion that doesn’t go away with sleep. And because symptoms creep in slowly, many wait years before getting tested. Blood tests for muscle enzymes like CK, muscle biopsies, and EMGs are the real diagnostic tools—not guesswork.
This collection of articles doesn’t just list drugs or symptoms. It connects the dots between myositis and the broader world of autoimmune disease, medication side effects, and how other conditions like lupus or thyroid disorders can overlap. You’ll find real stories about managing flares, avoiding dangerous drug interactions, and what works when standard treatments fail. Whether you’re newly diagnosed, caring for someone with myositis, or just trying to understand why your muscles won’t cooperate, these posts give you the facts without the fluff.