Protein Intake for Kidney Disease: What You Need to Know
When you have kidney disease, a condition where the kidneys lose their ability to filter waste and excess fluids from the blood. Also known as chronic kidney disease, it means your body needs careful handling of what you eat—especially protein. Too much protein can force your kidneys to work harder, speeding up damage. Too little can leave you weak, losing muscle, and more prone to infections. Finding the right balance isn’t about cutting protein completely—it’s about getting just enough to keep you strong without overloading your kidneys.
Protein intake for kidney disease is one of the most talked-about but misunderstood topics in renal nutrition. The way your body breaks down protein creates waste products like urea, which healthy kidneys easily remove. When kidneys are damaged, that waste builds up, causing fatigue, nausea, and further decline. That’s why doctors often recommend a low protein diet, a structured eating plan that limits protein to 0.6–0.8 grams per kilogram of body weight daily. For someone weighing 70 kg, that’s about 42–56 grams of protein a day—less than most people think. You don’t need to go vegan or avoid meat entirely. Instead, you swap large portions of beef or chicken for smaller servings, and fill the rest with vegetables, healthy fats, and controlled carbs.
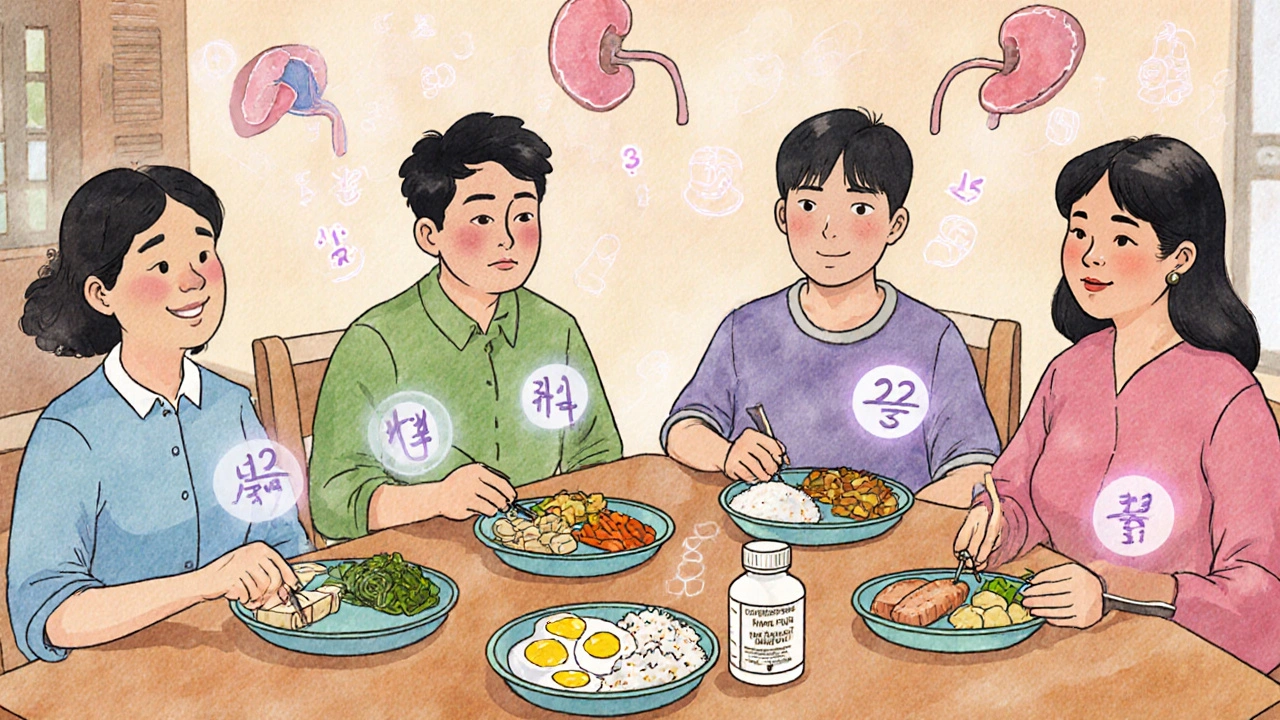
Not all proteins are equal. Animal proteins like eggs, milk, and meat create more waste than plant proteins like beans, lentils, and tofu. But plant proteins aren’t always easy to digest or complete—they lack some essential amino acids. The trick? Combine them. A little rice with beans gives you a full protein profile without overloading your kidneys. Some people also use specialized renal supplements that provide essential amino acids without the extra waste. These aren’t magic pills, but they can help when food alone isn’t enough.
What about people on dialysis? That’s a different story. If you’re on hemodialysis or peritoneal dialysis, your body loses protein during treatment. You might actually need more protein—not less—to stay strong and heal. That’s why your diet plan changes based on your stage of kidney disease, your treatment, your weight, and your muscle mass. One size does not fit all.
Monitoring your protein isn’t just about counting grams. It’s about watching how you feel. Are you tired all the time? Losing muscle? Getting sick more often? These are signs your protein intake might be off. Blood tests like serum albumin and BUN help your doctor track whether you’re on the right track. And yes, you can still eat delicious meals. Think grilled salmon with roasted veggies, a tofu stir-fry with brown rice, or a small chicken breast with mashed cauliflower instead of potatoes.
The goal isn’t to deprive yourself. It’s to protect your kidneys so you can stay active, feel better, and avoid complications like fluid buildup, high blood pressure, or heart problems. Many people with kidney disease live well for years by getting protein right—not by avoiding it, but by managing it smartly.
Below, you’ll find real, practical advice from people who’ve walked this path—whether it’s how to read food labels, what meals work best, how to handle cravings, or when to ask for a dietitian’s help. These aren’t guesses. They’re tested strategies from patients and providers who know what works when your kidneys are on the line.