Rheumatoid Arthritis Drugs: What You Need to Know
When dealing with rheumatoid arthritis drugs, medications used to treat the autoimmune joint disease rheumatoid arthritis. Also known as RA medicines, they aim to reduce inflammation, prevent joint damage, and improve quality of life.
One of the biggest breakthroughs in recent years is the rise of Disease-modifying antirheumatic drugs (DMARDs), agents that slow or stop the disease process rather than just masking pain. Classic DMARDs such as methotrexate, sulfasalazine and leflunomide have become the cornerstone of early therapy because they can halt joint erosion when started promptly.
Main categories of rheumatoid arthritis drugs
Biologic agents, protein‑based medicines that target specific immune pathways like TNF‑α, IL‑6, or B cells entered the scene after DMARDs and changed the treatment landscape for patients with moderate to severe disease. By binding to inflammatory cytokines or cells, biologics can dramatically reduce swelling and even achieve remission in many cases.
More recently, Janus kinase (JAK) inhibitors, small‑molecule pills that block intracellular signaling pathways involved in inflammation have given doctors an oral alternative to injectable biologics. Drugs like tofacitinib and upadacitinib work quickly and are often used when patients cannot tolerate biologics.
While DMARDs, biologics, and JAK inhibitors target disease mechanisms, non‑steroidal anti‑inflammatory drugs (NSAIDs), analgesics that relieve pain and swelling without altering the disease course remain essential for day‑to‑day symptom control. Corticosteroids, though powerful, are usually prescribed short‑term because of their side‑effect profile.
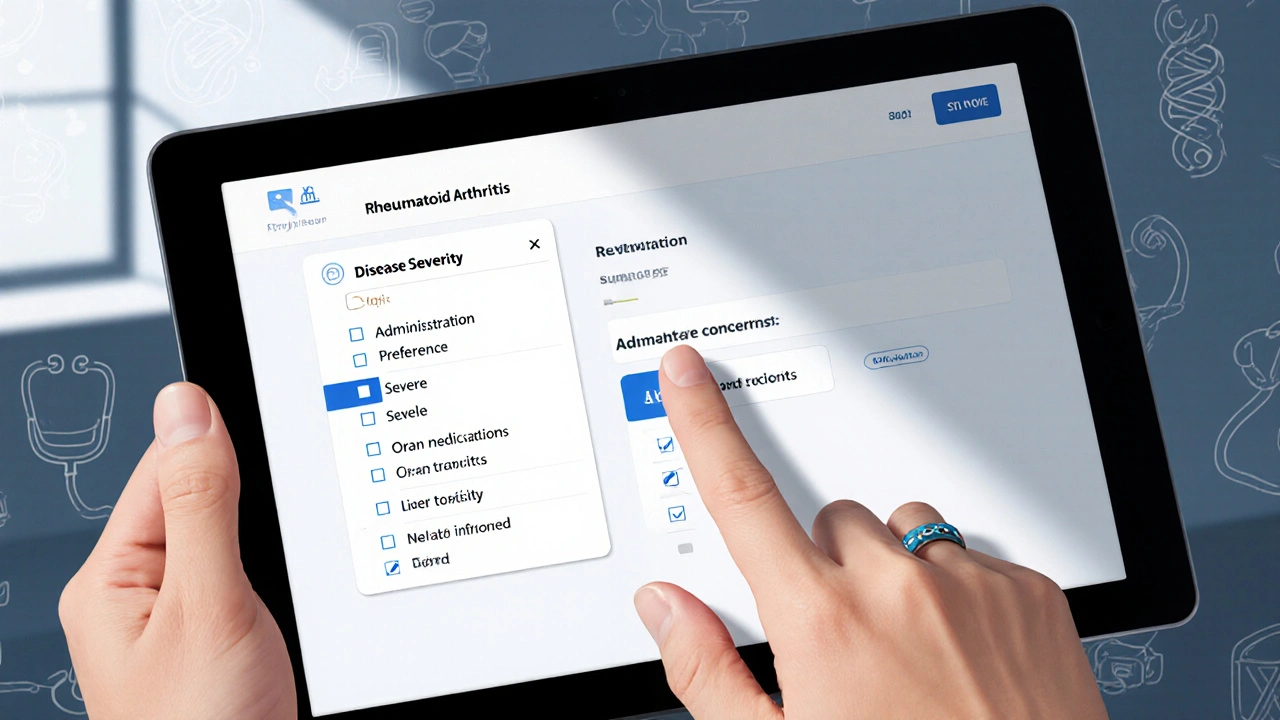
Choosing the right rheumatoid arthritis drugs isn’t a one‑size‑fits‑all decision. Rheumatologists assess disease activity scores, imaging results, and patient preferences before building a regimen. For early‑stage patients, a low‑dose methotrexate plus NSAIDs may be enough. When the disease progresses, a biologic or JAK inhibitor is often added to the mix.
Monitoring is a continuous part of therapy. Blood tests check liver function, blood counts, and kidney health, while regular joint exams gauge how well the medication is protecting the cartilage. Adjustments happen based on lab trends and how the patient feels—sometimes a dose tweak, other times a switch to a different drug class.
What matters most is acting early. Studies show that starting effective therapy within the first few months can prevent irreversible joint damage and keep patients active. Empowering patients with clear information about each drug class helps them participate in treatment choices and stick with the plan.
Below you’ll find a curated collection of articles that dig deeper into each drug category, compare options, and offer practical tips for safe use. Whether you’re just diagnosed or looking to fine‑tune an existing regimen, the resources ahead cover the full spectrum of rheumatoid arthritis drugs.