Topical Antibiotics: What They Are, How They Work, and When to Use Them
When you get a small cut, scrape, or infected pimple, your first thought might be to grab a topical antibiotic, a medication applied directly to the skin to kill or slow the growth of bacteria. Also known as antibiotic ointments or creams, they’re meant to prevent infection in minor wounds—but they’re not always necessary, and overuse can do more harm than good. These products, like Neosporin or Bacitracin, are designed for surface-level bacterial infections, not deep tissue or systemic issues. They work by targeting common skin bacteria like Staphylococcus and Streptococcus, but they don’t touch fungi or viruses. That’s why using them for athlete’s foot or a cold sore won’t help—and might make things worse.
One big problem? antibiotic resistance, when bacteria evolve to survive exposure to drugs meant to kill them. This isn’t just a hospital issue—it’s happening on your bathroom counter. Using topical antibiotics too often, especially for minor issues that would heal on their own, gives bacteria the chance to adapt. Studies show that over-the-counter topical antibiotics contribute to resistant strains like MRSA, especially when people use them daily for acne, razor bumps, or even dry skin. And here’s the catch: if you develop resistance to a topical antibiotic, it can make future infections harder to treat—even with oral drugs. That’s why many doctors now recommend simple cleaning and moisturizing over antibiotic creams for minor cuts. Clean water and petroleum jelly often do the job better and safer.
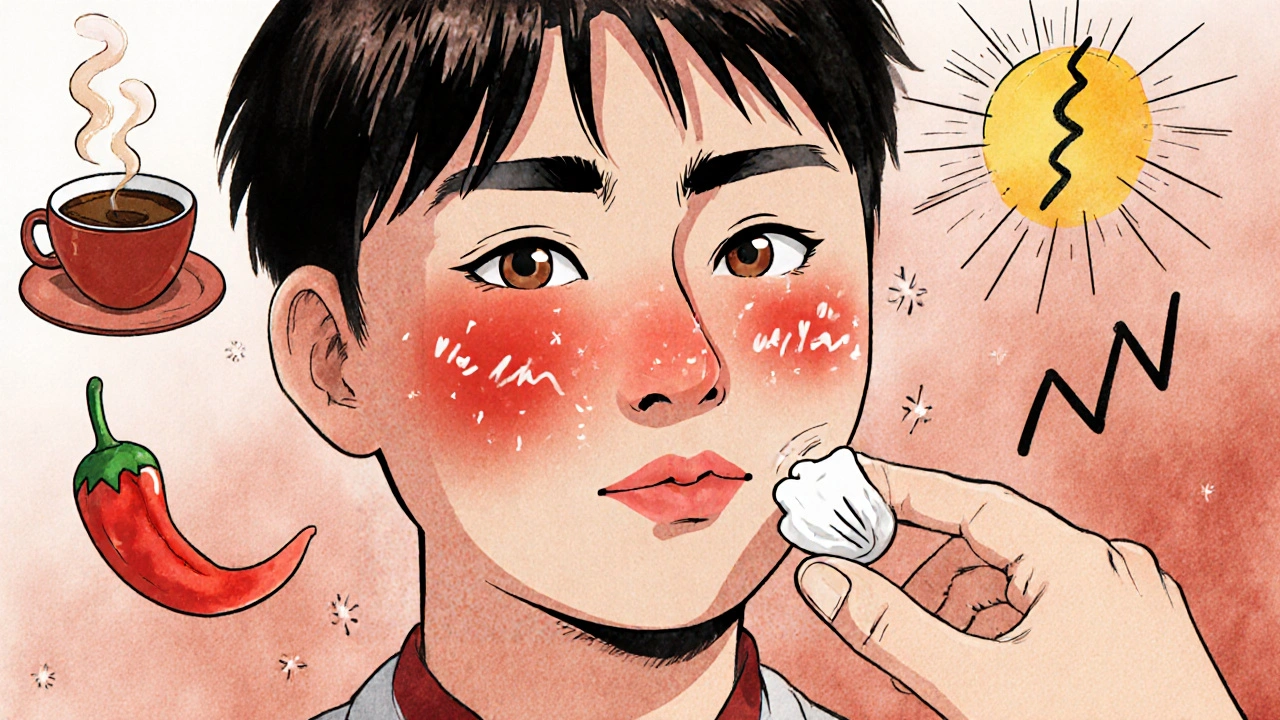
Not all skin problems need antibiotics at all. fungal infections, like athlete’s foot or yeast rashes, require antifungal treatments, not antibacterial ones. Many people confuse red, itchy skin for a bacterial infection and reach for Neosporin, when what they really need is clotrimazole or terbinafine. Even bacterial skin conditions like impetigo or folliculitis sometimes need prescription-strength topical treatments, not the stuff you buy at the drugstore. And if your skin issue is spreading, painful, or doesn’t improve in a few days, you’re likely dealing with something that needs professional care—not a tube of ointment.
There’s also a timing issue. Applying topical antibiotics to large areas, deep wounds, or burns can trap moisture and delay healing. They’re not meant for chronic conditions like eczema or psoriasis—those need different tools entirely. Even when used correctly, they can cause allergic reactions. Polymyxin B and neomycin, two common ingredients, are among the top causes of contact dermatitis from over-the-counter products.
So what should you do? For a tiny scrape, wash it with soap and water, pat it dry, and cover it with a bandage. Skip the antibiotic unless the wound is visibly dirty or you’re at high risk for infection. If you’re unsure, wait 24 hours. If it’s red, swollen, or oozing after that, see a provider. For acne, rosacea, or recurring rashes, talk to a dermatologist—there are far better options than generic antibiotic creams. And never use leftover antibiotics from a previous infection. That’s how resistance starts.
Below, you’ll find real-world guides on how topical antibiotics fit into broader treatment plans, when they’re actually useful, and how to avoid the traps that come with overuse. From skin care routines to understanding resistance, these posts give you the facts—not the hype.