Vasculitis: Causes, Symptoms, and Treatment Options Explained
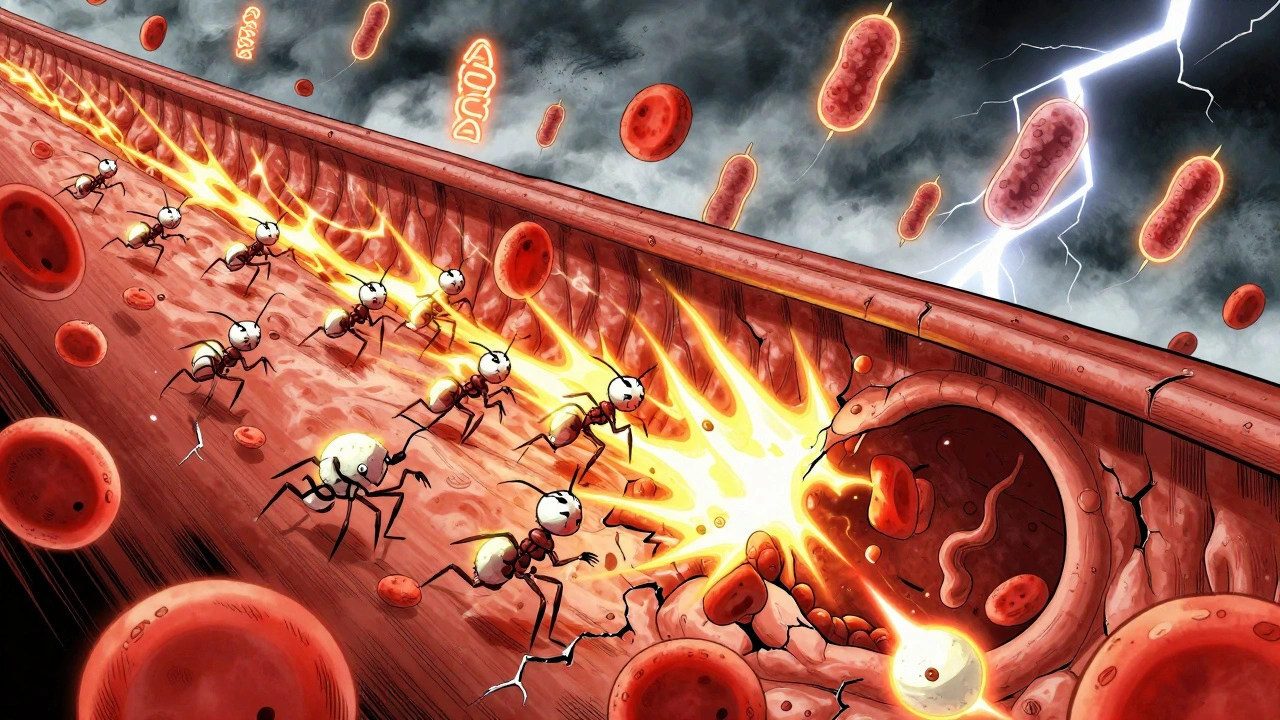
When your vasculitis, an autoimmune condition where the body attacks its own blood vessels. Also known as inflammatory vasculopathy, it can narrow or block vessels, cutting off blood flow to vital organs like the kidneys, lungs, or skin. This isn’t just a rash or a bad headache—it’s your immune system going rogue, and the damage can be serious if left unchecked.
It’s not one disease but a family of disorders. Giant cell arteritis, a type that targets large arteries near the head, often causing severe headaches and vision loss hits older adults hard. Granulomatosis with polyangiitis, formerly called Wegener’s, affects the sinuses, lungs, and kidneys. Then there’s polyarteritis nodosa, a systemic form that strikes medium-sized arteries and can cause abdominal pain, nerve damage, or high blood pressure. Each type has its own pattern, but they all share one thing: inflammation tearing through the walls of your blood vessels.
What causes it? No one knows for sure. But it often shows up after an infection, or alongside other autoimmune conditions like lupus or rheumatoid arthritis. Some people develop it after taking certain medications, while others have no clear trigger at all. Symptoms vary wildly—fatigue, fever, weight loss, numbness, skin ulcers, or even sudden kidney failure. If you’ve had unexplained pain or fatigue that won’t go away, and your doctor can’t find a simple explanation, vasculitis might be on the list.
Treatment isn’t one-size-fits-all. Steroids like prednisone are often the first line—they calm the immune system fast. But long-term use brings risks: bone loss, weight gain, diabetes. That’s why doctors pair them with drugs like cyclophosphamide or rituximab, which target the immune cells causing the damage. Newer biologics are showing promise, especially for people who don’t respond to older meds. And it’s not just about pills—monitoring organ function, managing blood pressure, and catching flares early can mean the difference between staying active and facing permanent damage.
You’ll find real stories here—not theory, not textbook summaries. People who lived through vasculitis flares, managed side effects from steroids, figured out what tests actually matter, and learned how to tell if a new symptom is a flare or just a cold. We cover how doctors diagnose it with blood tests, biopsies, and imaging. We explain why some treatments work better for certain types. And we show you what recovery really looks like—because this isn’t just about stopping inflammation. It’s about getting your life back.